Part 2 - Meet the physicians stonewalling safe supply
Where there's smoke: reaching deeper into commercial interests of physician signatories to an open letter blasting safe supply.

Let’s recap Part 1: seventeen addiction physicians signed an open letter on September 25, addressed to Minister of Mental Health & Addiction Ya’ara Saks, titled “RE: Unsupervised Free Government Funded Hydromorphone Programs.”
Although the letter made sweeping claims about the dangers of safe supply, it cited no evidence against these programs, which are designed to reduce people’s contact with the unregulated and deadly street fentanyl supply. The letter dismissed the rapidly emerging health and safety evidence in favour of these programs.
The letter also failed to declare more than four fifths of the physicians’ commercial interests, each of which could skew their views on safe supply. It turns out that 15 of the 17 physicians hold commercial interests that could hypothetically, through political or financial channels, muddy their involvement with safe supply advocacy.
Of these 15, only Dr. Harry Vedelago, Dr. Alan Brookstone and Dr. Clement Sun mentioned commercial interests in their bio. Four signatories did not provide bios.
While writing Part 1, I fell short of identifying commercial interests for Dr. Mel Kahan, Dr. Launette Rieb, Dr. Benjamin Jang and Dr. Mehdi Ispahany. I’ve since learned Dr. Jang and Dr. Ispahany hold relevant commercial interests. Dr. Rieb asserted a lack of conflicts in her presentation to the Alberta Safe Supply Committee in 2022 (a government-funded exercise in public dissuasion), and Dr. Kahan provided a written submission to the Committee. We’ll revisit this in Part 3.
Dr. Mehdi Ispahany and Dr. Benjamin Jang
Dr. Clement Sun was cited in Part 1 as the owner of the ACT Addiction Clinic chain.
What I missed at the time was that two additional letter signatories are commercially involved with this company: Dr. Ispahany and Dr. Jang both list an ACT Clinic in Toronto as their primary practice addresses.
Dr. Ispahany’s additional practicing addresses are Aurora IDA Pharmacy, Bodystream Medical cannabis prescribing clinics in Thunder Bay and North Bay, and a building in Newmarket with one or two pharmacies and walk-in clinics.
Dr. Jang’s additional practicing addresses are an ACT Clinic in Kitchener and a rather shabby-looking ACT Clinic in Peterborough. Interestingly, Dr. Jang’s professional corporation listing these addresses was only established in 2022, although he did appear to complete his medical residency in Family Medicine in 2013.
The Star’s database of Ontario doctors
The Toronto Star released a database in 2019 showing physician billing for the 2017-18 tax year. It comes with a disclaimer:
“These are payments for fee-for-service only. That is just more than half the $12.6 billion Ontario paid physicians in 2017-18. Many doctors, particularly family doctors, are paid in other ways, such as per patient or by salary, amounts that are not included here. Total billings are not the same as income. Overhead costs come out of billings and can include expenses for staff, offices, equipment and supplies. They can be significant, depending on specialty and practice.”
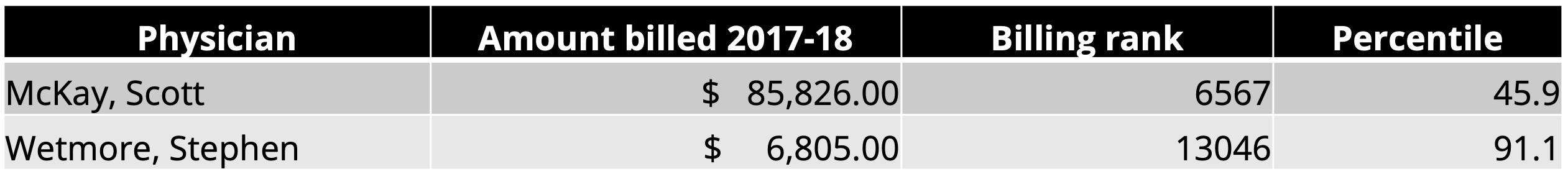
I’ve put together a table showing the eight Ontario signatories to the open letter with the amount they billed in 2017-18, how this amount ranks among 14,314 family/general practitioners, and their billing percentile (top X%):
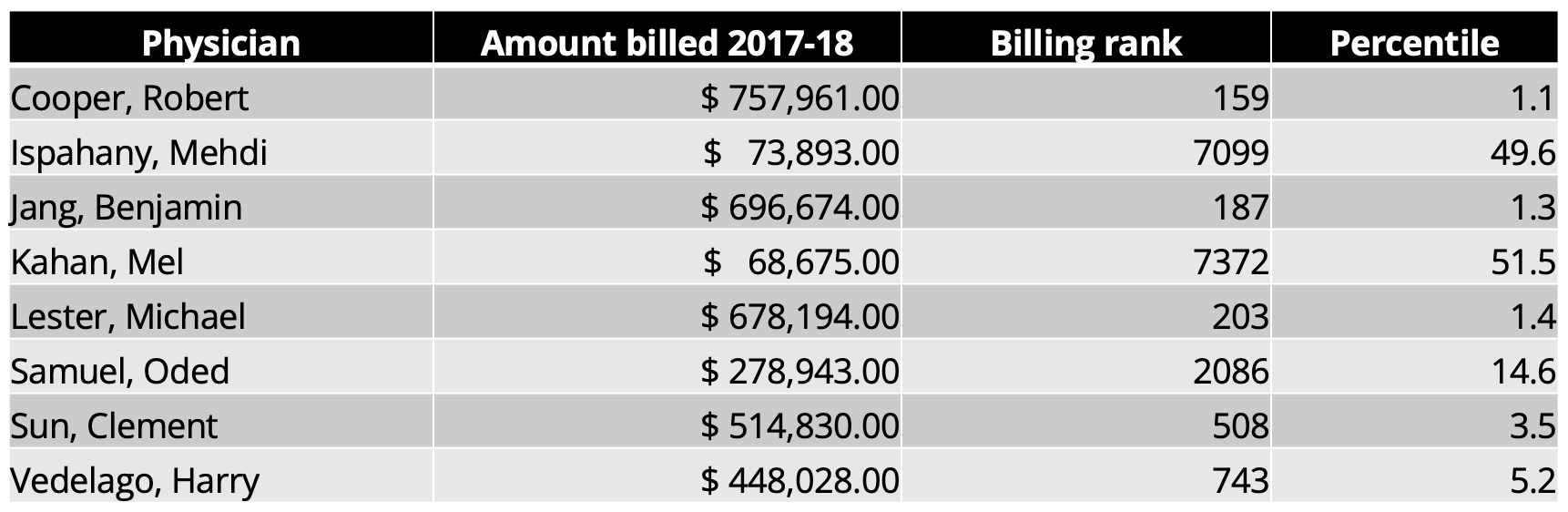
Congratulations to Dr. Kahal for being the only billing physician below the average. As Medical Director at META:PHI, Dr. Kahan likely conducts very little clinical work, so his ranking makes sense. Dr. Oded billed in the top 15% but had not yet opened his apparent virtual prescribing business, SkriptMD (see Part 1). Dr. Ispahany, middle of the pack in billing for 2017-18, was detailed above.
Given the Star’s note above about overhead costs, it’s worth pointing out what a combined $1,285,397 annual billing in 2017-18 might be yielding from the three ACT Clinic prescribers listed in the table above:

Because many of these physicians show up in defence of Alberta Government policy decisions, with Alberta Safe Supply Committee in 2022 being of recent importance, I looked up the two additional Ontario physicians who presented or submitted to the committee (more on this in Part 3). Both billed near the top 5% among family/general practitioners.

As a limited control group that shows how steep this curve is, I searched the two physicians Dr. Koivu works with at St. Joseph’s Health Care London. They ranked near the middle and near the bottom in billing.
I’ll repeat that these are not take-home incomes, because each of these private practices will have overhead and staffing costs to cover. But it also does not account for salaries or services for which billing does not occur.
Also noteworthy is that in 2018, Dr. Mel Kahan was raising the alarm about people that seem an awful lot like some of his co-authors on last week’s open letter:
“more than half of the methadone distributed in the province in 2014 was prescribed by just 57 doctors, most of whom worked in high-volume clinics that provide little in the way of counselling or physician support … it concluded that the top 10 per cent of methadone prescribers billed for an average of nearly $650,000 in services related to methadone in 2014, nearly twice the average gross annual billings for Ontario physicians.
Meldon Kahan, a co-author of the study…” [emphasis mine]
From: U.S. addiction-treatment firm buys Ontario methadone clinics by Kelly Grant, Globe & Mail, March 8 2018
While we’re talking money, I’ll emphasize that the 10 federally funded safe supply pilots require prescribing physicians to be on salary. This means that in these pilots ongoing across the country (notably not in Alberta), no physician is profiting from opioid prescribing. It doesn’t matter how much, how little, or which brand they prescribe, they get paid the same amount.
These salaries are set through negotiations between provincial medical associations (doctors’ unions) and the provincial governments. Safe supply-piloting doctors in Canada cannot profit from greater opioid prescribing even if they try.
For that matter, it’s worth noting two points Dr. Gillian Kolla made via Twitter, in response to a not-so-subtle accusation (and tired trope) by self-described “recovery physician” Dr. Lori Regenstreif, who also happens to use a racial slur as a Twitter handle, that safe supply proponents are funded by Purdue:
“If I was going to pick a conflict-of-interest conspiracy trail of crumbs to follow, it would be to scrutinize the role of Purdue Pharma in the promotion of Dilaudid® tablets in any health care or harm reduction setting. 🤔” - Dr. Regenstreif via Twitter

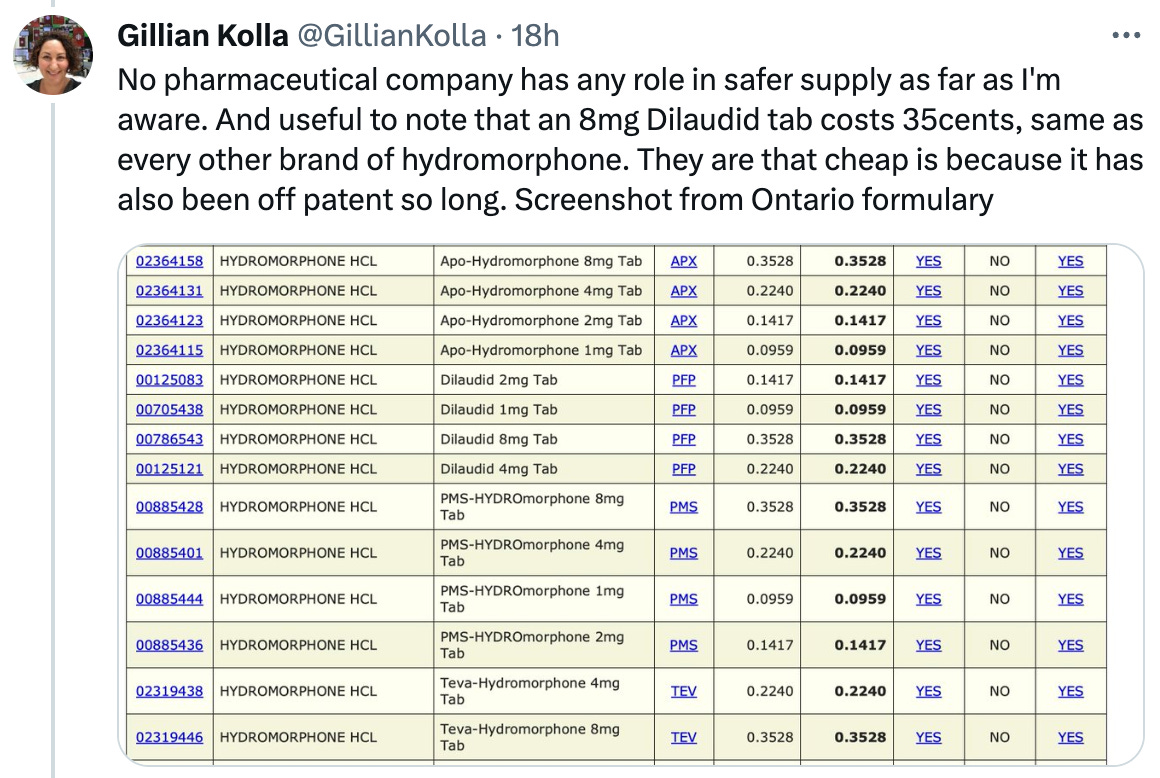
Dilaudid lost its patent and now costs $0.35 per 8mg tablet. According to a physician I spoke with, the main reason physicians still prescribe the Purdue version is that it dissolves better than the generic version for injection. That’s a form of harm reduction.
Meanwhile, Sublocade (injectable buprenorphine sold by Indivior) is going for $550 per injection, and each injection lasts about a month.
Media coverage
On September 29 (a day after I published Part 1), Tyler Dawson at the National Post covered the open letter. The piece ignored the vested interests of the signatories, with the exception of Dr. Clement Sun’s ownership of ACT Addiction Clinic chain, disclosed in the letter. Seven of the first eight paragraphs described the letter and quoted its proponents. However, the article then featured rebuttals of each point made in the letter by Dr. Gillian Kolla and Dr. Paxton Bach, neither of whom own companies, and cited various statements in defence of safe supply by BC officials.
I’m surprised. Overall, it was a generally balanced and well researched piece.
Then on October 5, Adam Zivo entered with his targeted propaganda in National Post Comment, describing the letter as “yet another blow to the federal and B.C. governments, both of which are politically invested in safer supply’s success.”
Call these governments’ political investments what you will, but for the second time in six days, the Post failed to highlight the financial investments held by the letter’s authors.
Otherwise, I have yet to see any media outlet pick up this quickly necrotizing piece of medical history.
I’ll wrap up with something Dr. Melamed stated in her Alberta Safe Supply Committee presentation, which we’ll return to in Part 3:
“Addiction is a disease where you need a community. A therapeutic community plus your doctor who helps you, although we play a very small role in this…”
If doctors play a ‘small role,’ why are some billing $700,000 annually — the annual operating cost of many addiction treatment centres (most of which operate on minimum wage labour)? Why the unending op-eds and open letters to stall progress on unregulated drug poisoning?
It wouldn’t be a stretch to suggest they downplay their public role to maximize their private returns.
Did you enjoy this post or learn something cool? Please share it with a friend or copy the link and post it to social media!
Ready for Part 3?
Drug Data Decoded provides analysis on topics concerning the war on drugs using news sources, publicly available data sets and freedom of information submissions, from which the author draws reasonable opinions. The author is not a journalist.