Up next...'experts' debate the ethics of reducing drug poisoning deaths
A study in a top medical journal shows overwhelming positive impacts of regulated hydromorphone prescribing for people who use opioids in BC. Will the trolls keep yelling from their caves?
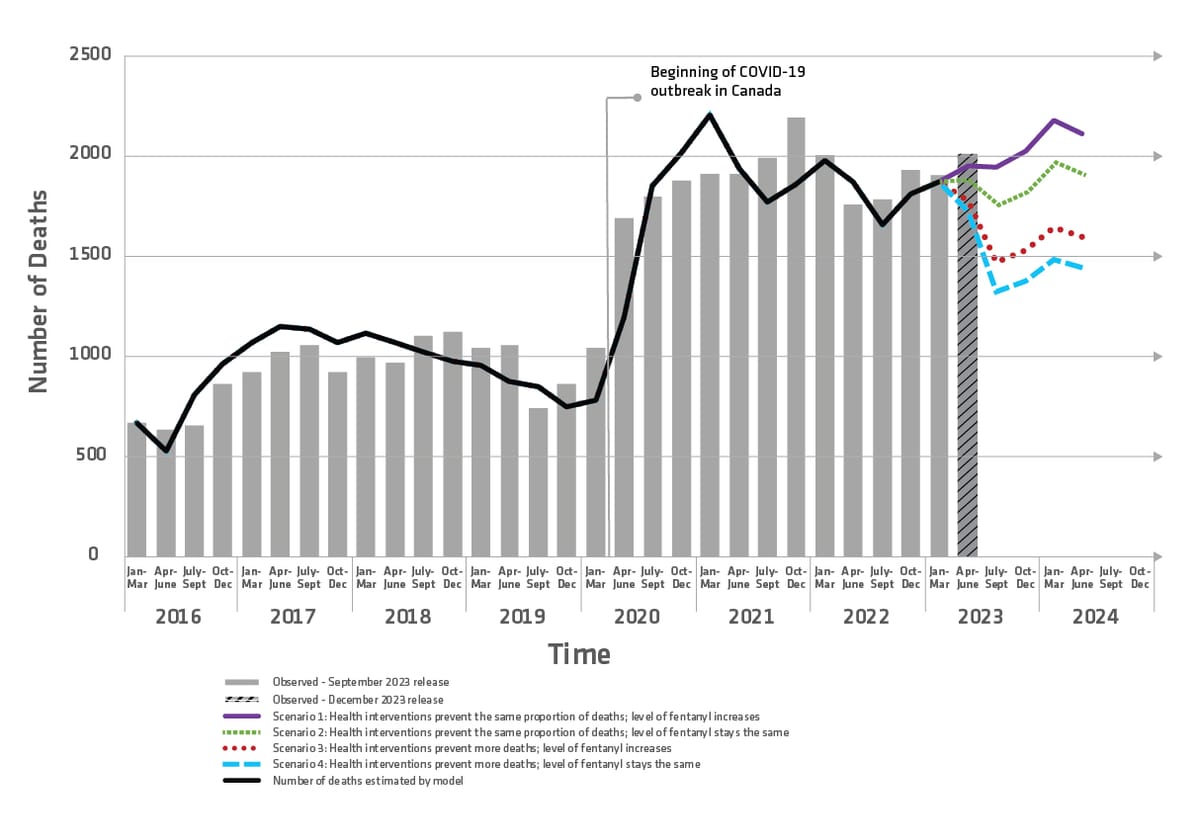
Tens of thousands are dead since opioid de-prescribing accelerated around 2015, but the scientific jury on safe supply just heard a loud closing argument.
After a year of sycophantic brow-beating by right-wing propagandists against safe supply prescribing, a large-scale study reveals massive decreases in death attributed to safe supply prescribing.
Published in a top medical journal on January 10 by a consortium of researchers from eight BC institutions, the study analyzed data from 5,356 people dispensed hydromorphone in prescribed safer supply programs in BC between March 2020 and August 2021. Outcomes for these people were compared within a larger group of 70,360 people diagnosed with ‘opioid use disorder’* using robust statistical methods.
Among people receiving 4 or more dispensations of hydromorphone in a given week, drug poisoning deaths were reduced by 89% over the subsequent week, while all-cause deaths were reduced by 91%.
Meanwhile, among people receiving one or more dispensations of hydromorphone per week, drug poisoning deaths were reduced by 55% over the subsequent week, while all-cause deaths were reduced by 61%.
Hydromorphone is not fentanyl. In relative potency, it lines up fairly closely with diacetylmorphine (heroin), while fentanyl is around 50 times stronger per unit of weight. So depending on purity and supply volatility, it makes it easier to get accustomed to higher-strength doses over time. Fentanyl is also much shorter-acting, meaning people often need to use it many times a day to maintain its effects.
The study was conducted before fentanyl prescribing was initiated in BC for people who use opioids. Alarmingly, safe supply prescribing nurse Corey Ranger noted that since the study period, safe supply prescribing has dropped precipitously in BC to around 4,331 individuals. This likely reflects a climate of fear among medical practitioners generated through political backlash by right-wing operators, which Drug Data Decoded has discussed at length.
The study also examined stimulant prescribing, and found no statistically significant impact on overdose/poisoning or all causes combined. This likely reflects the continued dominance of fentanyl in drug poisoning deaths.
Stimulant prescribing did relate to a drop in all-cause acute care visits. This could indicate the impact of simple contact with medical practitioners on people who use stimulants. Opioid prescribing showed no statistically significant impact on acute care visits.
This contrasts a 2023 study from London, ON showing a large decrease in emergency department visits related to safe supply prescribing between 2016 and 2019. The authors imply this discrepancy may in part be owing to the higher risk of acute care use among people with unstable shelter; as Ranger told Drug Data Decoded,
“If I were to interpret the data based on my experience working in these programs, I’d point to the study period having covered the first 18 months of the COVID pandemic. During this time, many people receiving prescribed safe supply were also provided temporary housing under local and provincial government pandemic programs. Another possibility for this discrepancy is that the Ontario safe opioid supply program, where the earlier study was based, includes significant wraparound care supports. These help reduce visits to emergency rooms by preventing bigger medical issues from developing out of smaller ones.”
It’s long past time for governments to step up
Despite earlier qualitative studies and advocacy by people in these programs insisting that they are saving lives, the BC health authorities have quietly allowed safe supply prescribing to slip by nearly 20%. This transpired through a political moment when BC Premier David Eby tried to push through drug re-criminalization (it was only a legal injunction led by Harm Reduction Nurses Association, Pivot Legal and Canadian Drug Policy Coalition that stopped Premier Eby’s bill).
Meanwhile, Alberta Premier Danielle Smith left off the conversation by informing us “We’re not doing safe supply.” Given the results of this study and others, Smith is really saying “We don’t care about the lives of people who use drugs.”
The public needs to hold politicians to account for standing on the wrong side of history—along with heartless police chiefs, spineless municipal councillors, and self-enriching physicians.
Join a rally on January 16 (Vancouver, Calgary, Nelson and London, England so far) in solidarity with safe supply and the Drug User Liberation Front as they enter the courtroom on the first day of their proceedings.
With clear evidence that your support underpins people’s Charter Section 7 right to life, liberty and security of the Person, who could argue against you?

*Another study serendipitously published a day earlier in the same journal describes the frequency of undeclared conflicts of interest among physicians who contributed to the latest revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). It reveals that 40% of contributors to the chapter on Substance Use Disorder held financial conflicts of interest that were undeclared. The authors argue that these conflicts should have been disqualifying for these contributors, as they undermine the credibility of diagnoses such as ‘substance use disorder’ or ‘opioid use disorder.’





