The Alberta Drug Model is a Christian institution: Part 3
Tough love, paternalism and cultural erasure in Alberta's 'recovery-oriented system of care.'
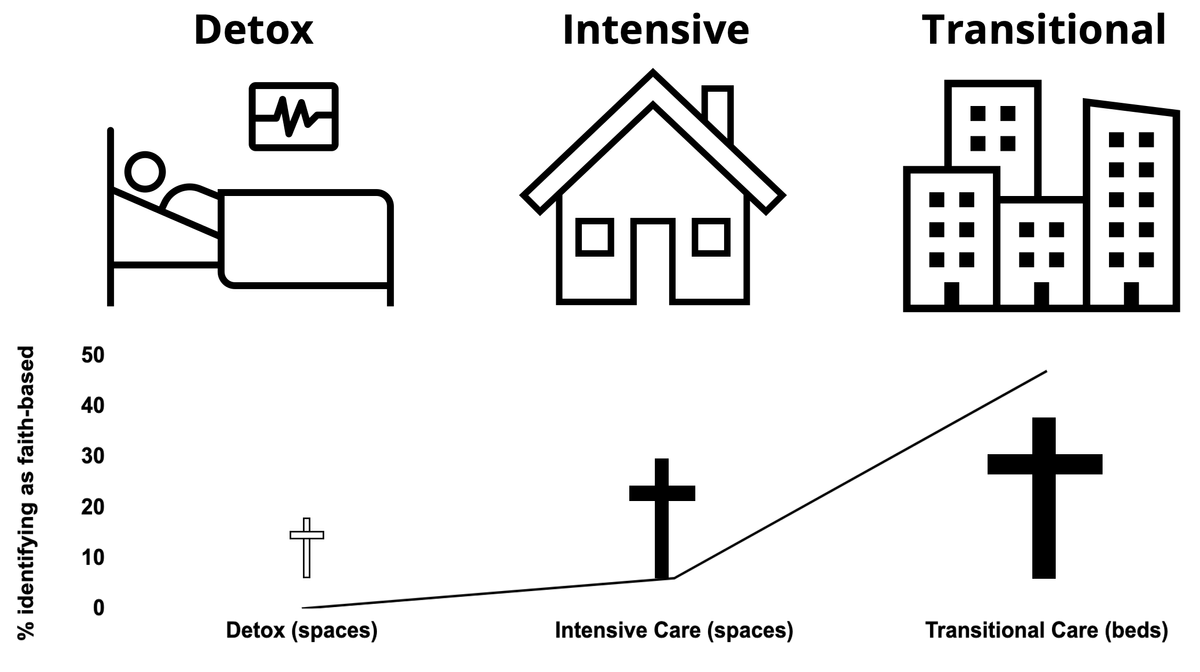
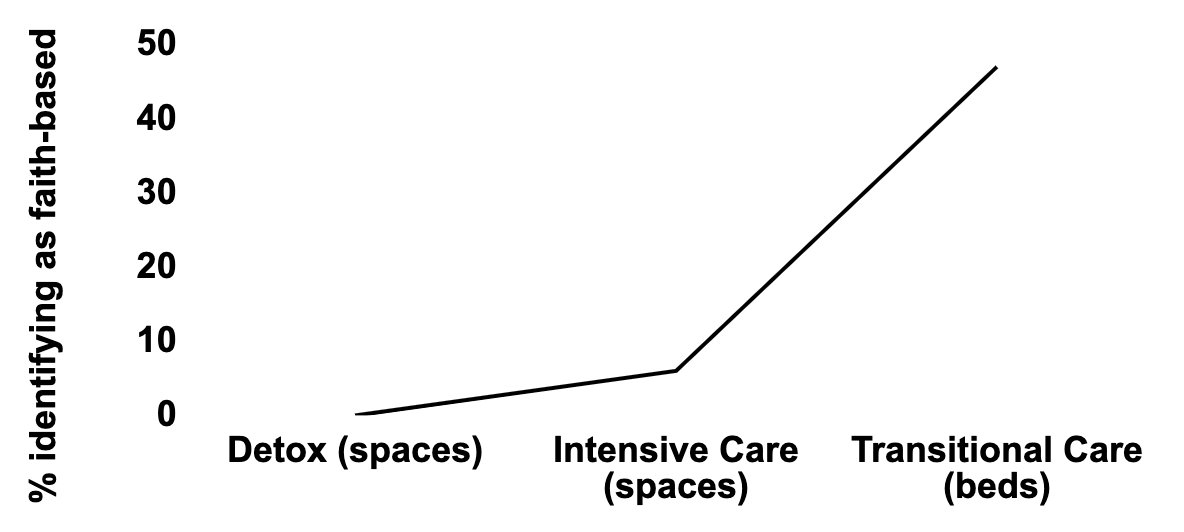
In Part 1, we discussed how Transitional or Supported Recovery programs in Alberta are dominated by Christian theology, which works its way through explicit faith-based programming as well as implicit 12-Step programming. As Maia Salavitz made clear in her recent New York Times piece, 12-Step is an abstinence model that has been determined by American courts to be religious in nature.
In Part 2, we examined how Detox programs fail to respond to the rapidly shifting drug supply and its consequences of polysubstance withdrawal. While there remain no public evaluation metrics for detox or other care programs, we have to accept the data as they stand: many people wind up back on the street supply rather than following through to sustained abstinence. The fact is, they are not being met where they’re at, even at this early step of substance use care.
Here in Part 3, we’ll land in the middle with the Intensive Care facilities, and look at how this publicly funded system, dominated by private institutions, may be operating as a funnel to Christian abstinence-based ideology and its intersections with tough love, paternalism and Indigenous cultural erasure.
First, let’s refresh the difference between beds and spaces. “Beds” is self-explanatory: the number of beds present in all facilities of a given category. “Spaces” contextualizes the annual potential use of beds based on length of programs. So a facility with 10 beds and a 36-day program would have 365 / 36 * 10 = 101.4 spaces.
For Transitional Care (Part 1), we looked at Beds because the program durations were too variable to extrapolate to Spaces. For Detox (Part 2) we based the data on Spaces and for this Part 3 instalment on Intensive Care, we’ll do the same.
The data are compiled from an AHS document summarizing the facilities and their offerings and formats. The document is not entirely complete, but I’ve filled in some gaps with calls to facilities. Look for more robust media coverage as journalists take more interest (media: feel free to request the document!).
Hypothesis: tough love, paternalism & cultural erasure
Alberta remains fertile ground for residential school denialism, open misogeny, and tough love. So it stands to reason that a field reinforcing century-old prohibitionist ideology might find common cause with these ways of thinking.
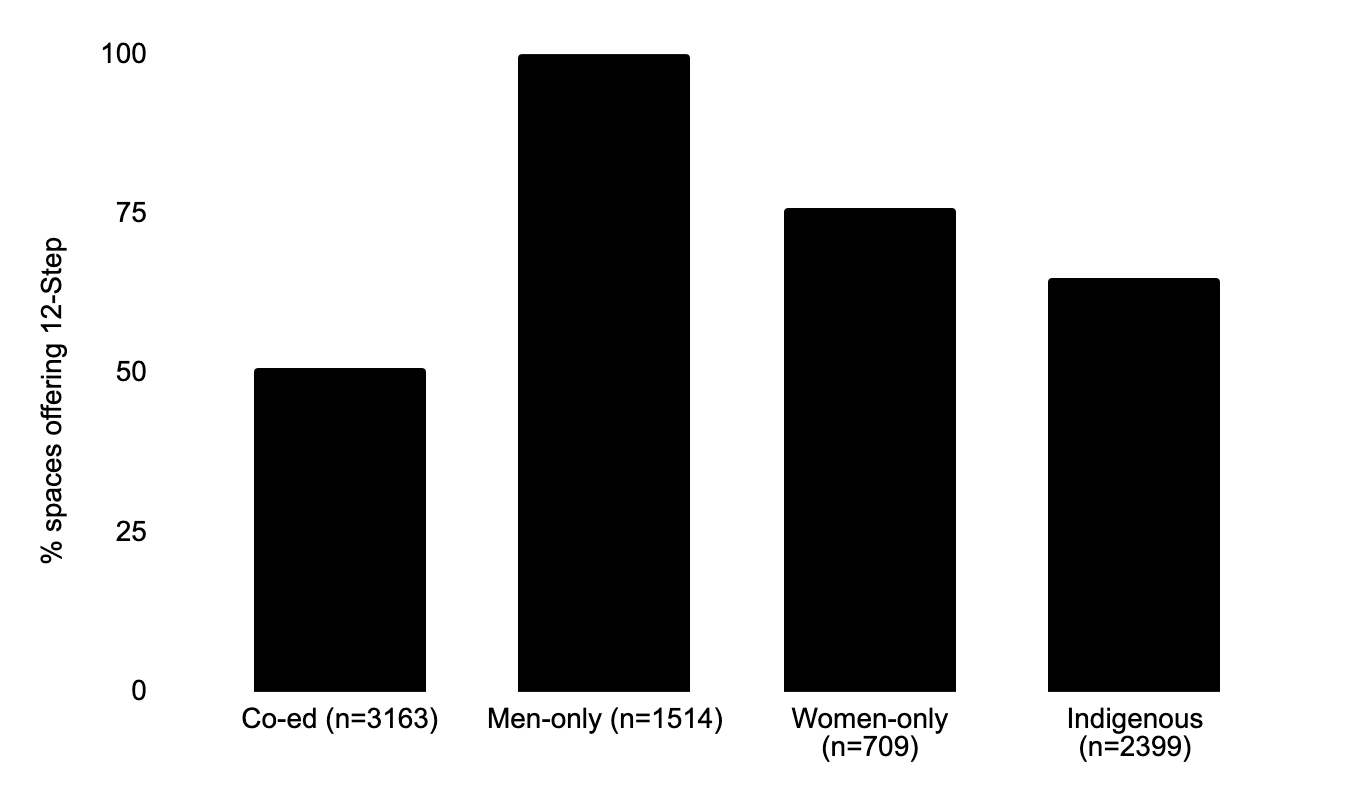
Part 1 described 12-Step abstinence programming as an implicit expression of Christian ideals in substance use care. Again: this doesn’t mean 12-Step can’t work for some people, or that it shouldn’t be available. But as faith-based programming shies away from scrutiny, we should keep turning stones to look for 12-Step under a secular façade.
Let’s go through the most interesting comparisons from the AHS facility data. The categories are co-ed, men-only, women-only and Indigenous, as delineated in the AHS document:
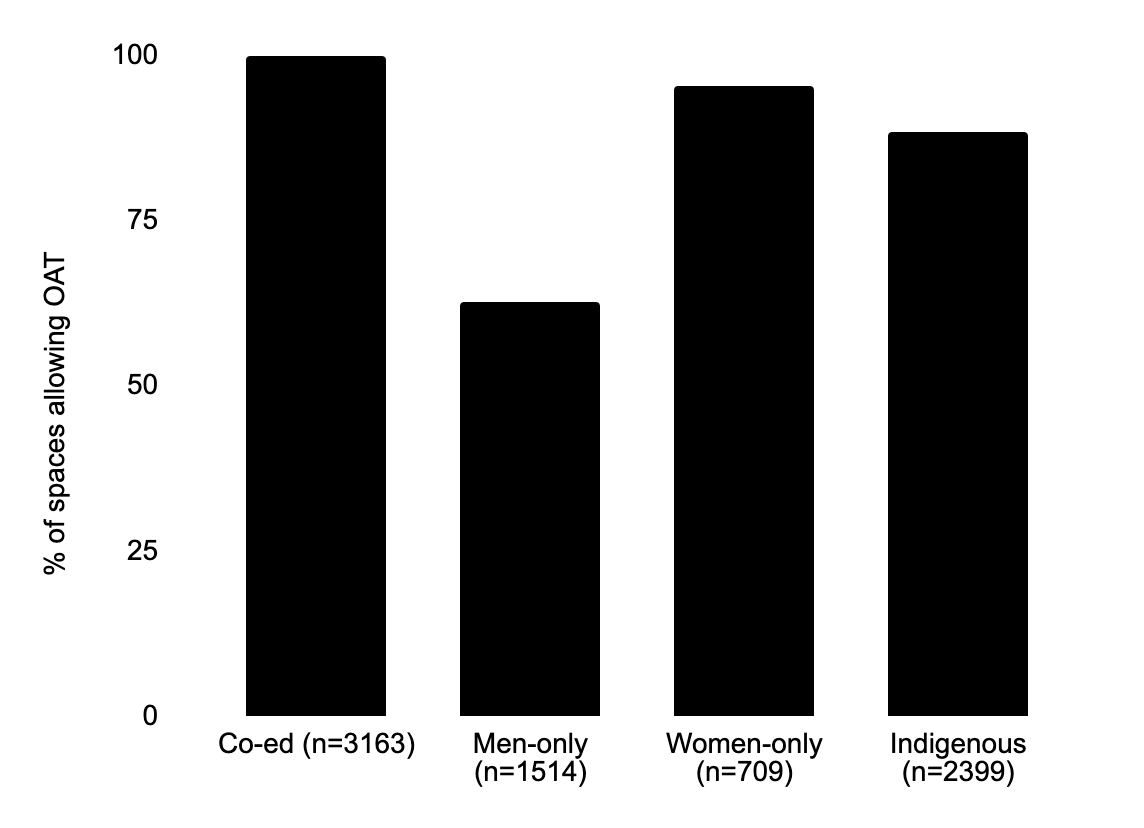
- Men-only spaces are far more likely to deny the use of opioid agonist treatments (OAT) like Suboxone, methadone and Kadian. This tough-love pattern is the result of a single large facility that seems to resist the increasing recognition of the value of these pharmaceuticals in managing substance use.
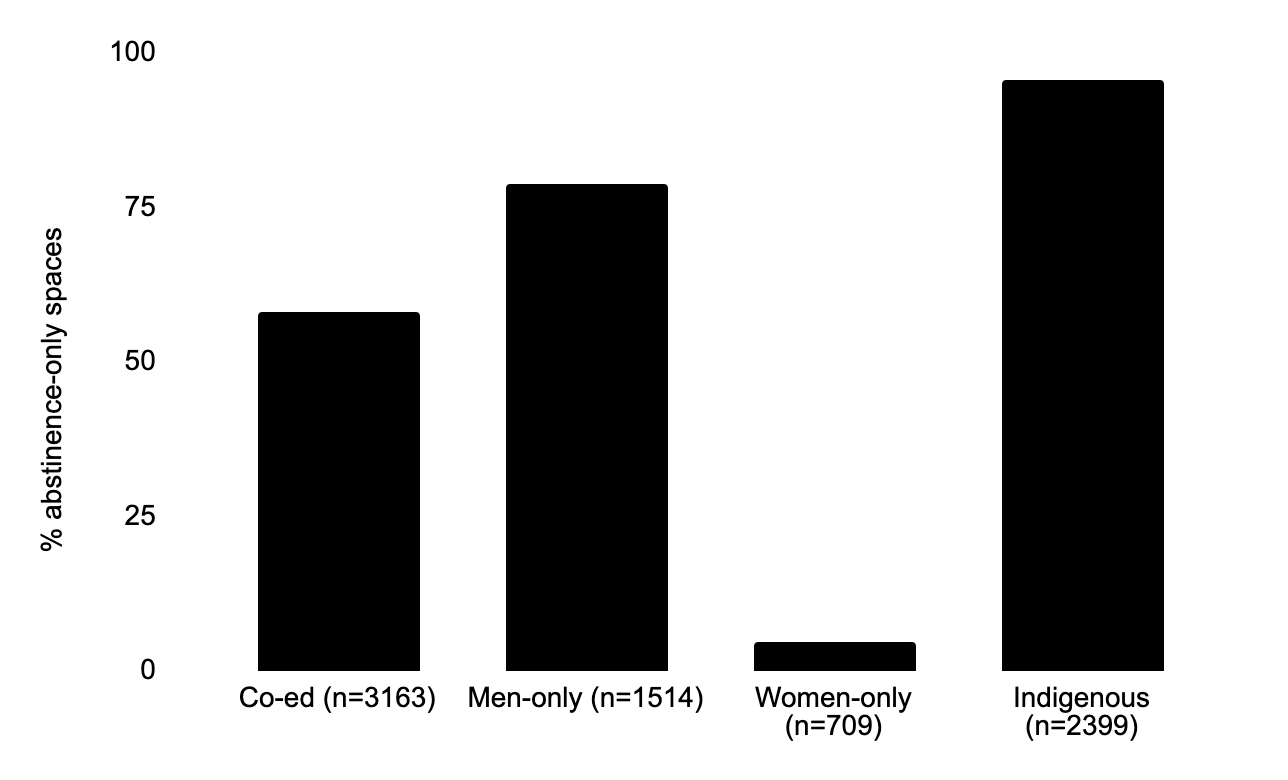
Related, Indigenous and men-only spaces are far more likely to be abstinence-only. It’s impossible to know how each program was established, and who framed them as abstinence-only, but assuming the Indigenous programs are designed and funded through the province, this looks an awful lot like tough love with a colonial accent. It’s also fascinating that the vast majority of women-only spaces are not explicitly abstinence-based.
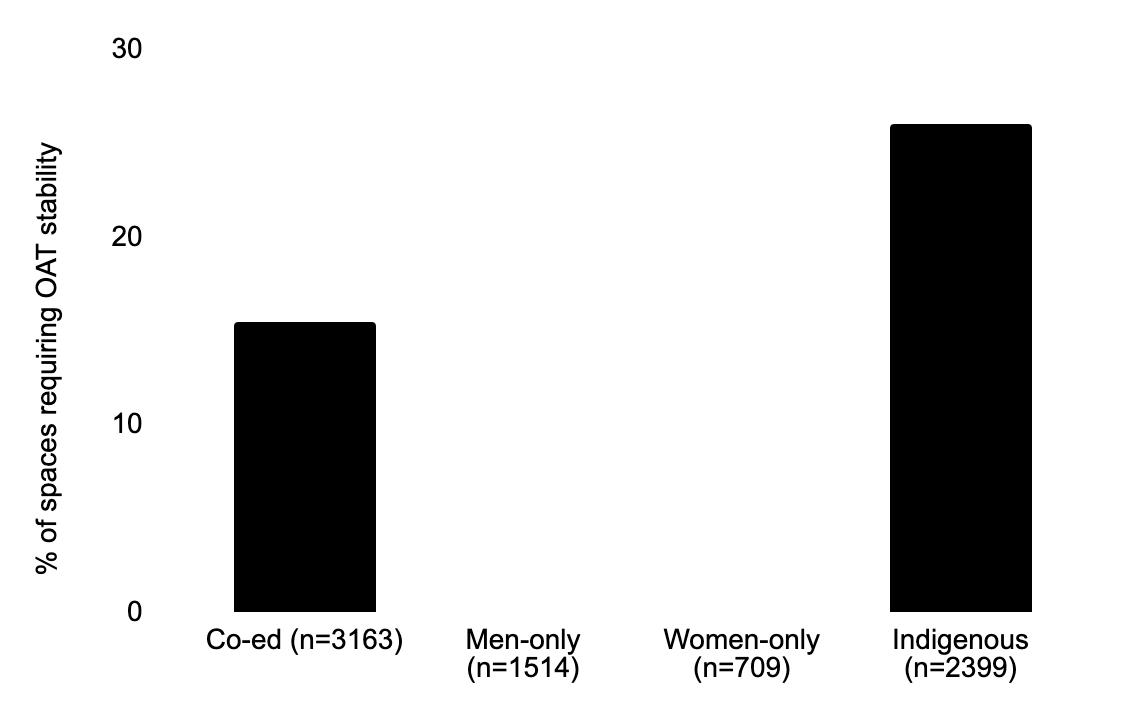
Indigenous spaces are far more likely to require a period of OAT stabilization before admission. I often hear about this being a technique for ‘weeding out’ people who are less likely to complete a program. In some cases, this could be used by programs to fluff up their statistics. In others, it could be a recognition that limited space should be triaged for those most likely to succeed.
Spaces that admit women are far more likely to restrict smoking. This rings of the type of structural misogeny that dismisses women’s needs not pertaining to pregnancy. Yes, smoking harms fetuses. But putting patients first means prioritizing comforts in a harsh care context.
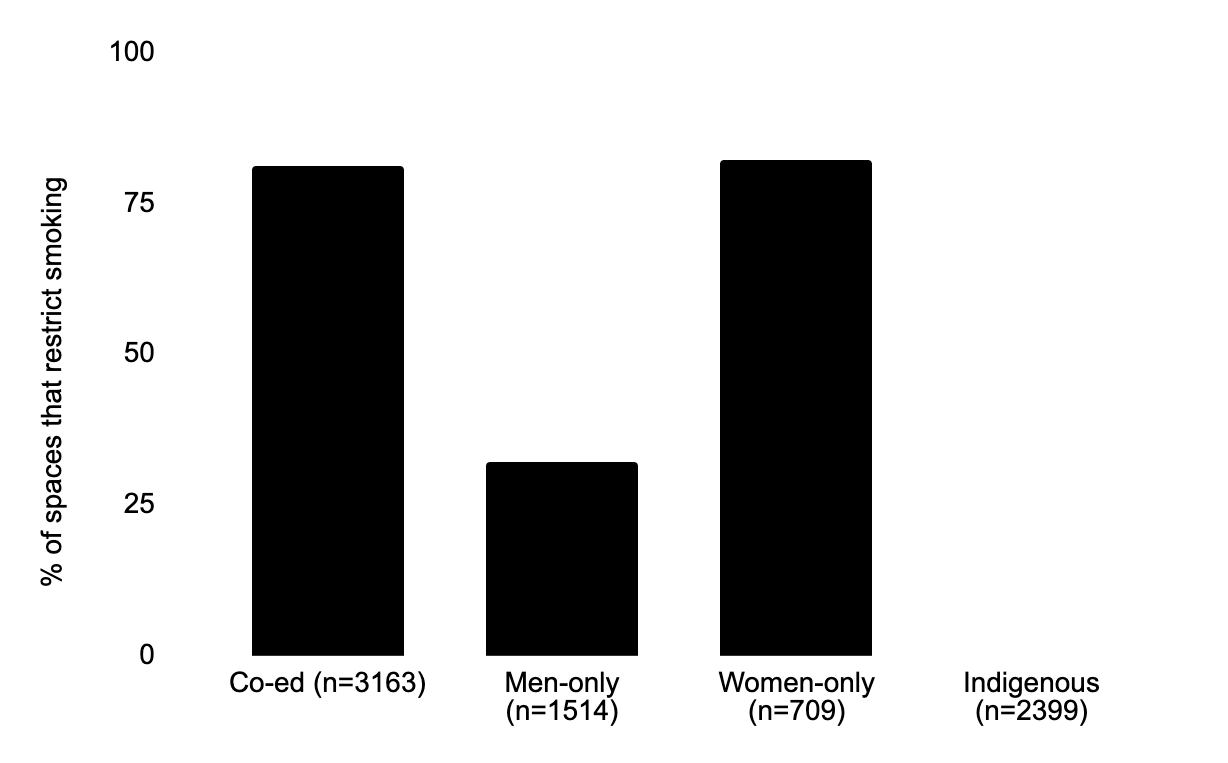
Interestingly, this pattern holds up among Transitional Care programs too (which don’t have an Indigenous categorization, so this likely skews the overall proportions lower): 27% of beds in women-only facilities are smoking-restricted, versus 13% in men-only facilities. However, there are no smoking restrictions at the co-ed facilities.
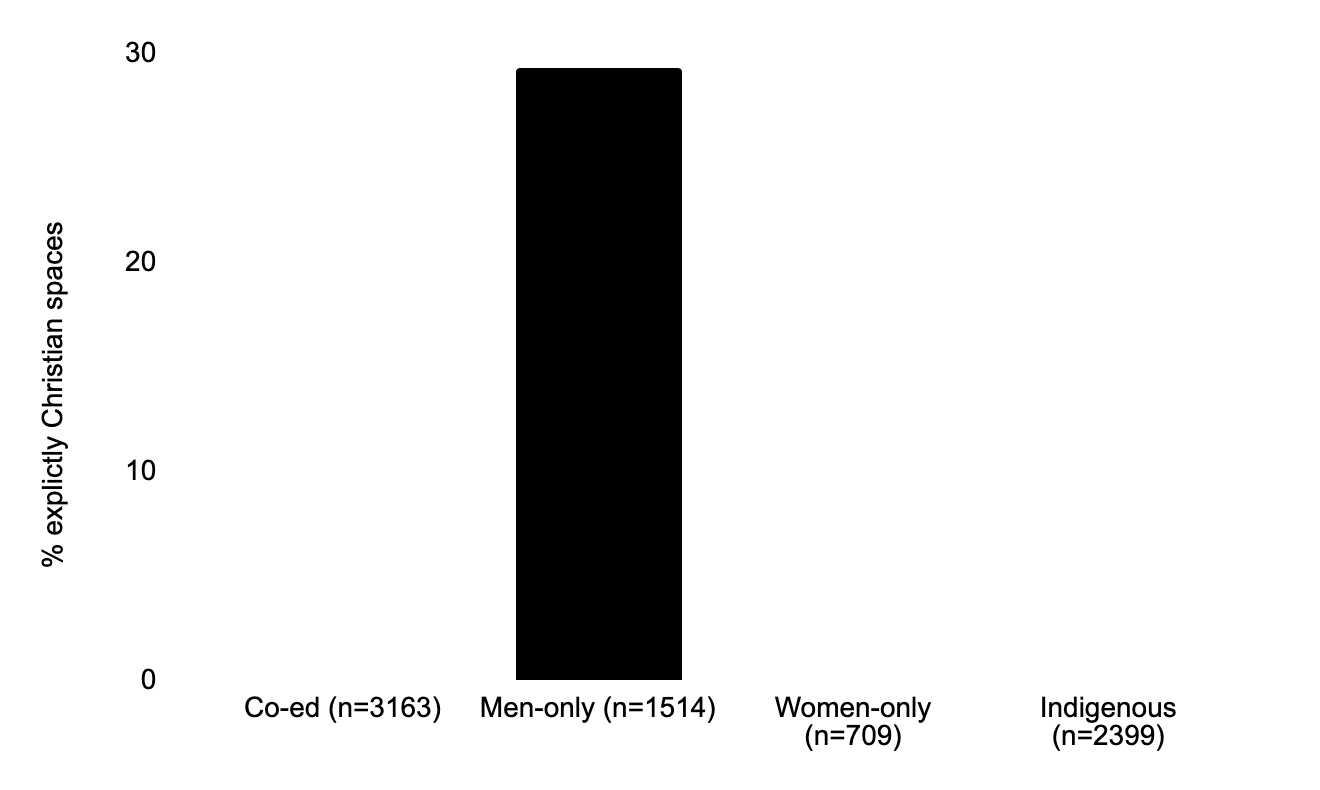
Finally, the only explicitly Christian spaces are men-only (owing again to a single large facility) but 12-Step is extremely prevalent in all space categories. Remember, 12-Step has been designated by American court proceedings as ‘religious in nature.’ Does this mean every facility providing 12-Step groups is religious? No. But if the primary programming is 12-Step, you can bet it’s getting a heavy dose of publicly funded faith.
So here’s what we can draw from the Intensive Substance Use Care facility data:
- Men-only spaces are far more likely to deny the use of opioid agonist treatments.
- Indigenous and men-only spaces are far more likely to be abstinence-only.
- Indigenous spaces are far more likely to require a period of OAT stabilization before admission.
- Spaces that allow women are far more likely to restrict smoking.
- The only explicitly Christian spaces are men-only, but 12-Step is frequently used in all space categories.
When we put this together with the Transitional Care (Part 1) and Detox (Part 2) data, does this suggest a system geared toward tough love, paternalism & cultural erasure of Indigenous peoples?
I think so.
Taken together, does the ‘treatment’ pipeline as a whole suggest a process by which vulnerable people are primed for religious indoctrination? I’ll leave that up to you.
Conclusion
In June, 2022 over 30 organizations co-signed an open letter to the UCP government asking for transparency on substance use care. We have yet to receive a response or details on the 50 evaluation criteria detailed in the letter.
Fortunately, the internal AHS document we’ve dissected through this series does help to answer several of the questions in the letter. An upcoming post will show how the present investigation has shed light on several of these missing criteria.