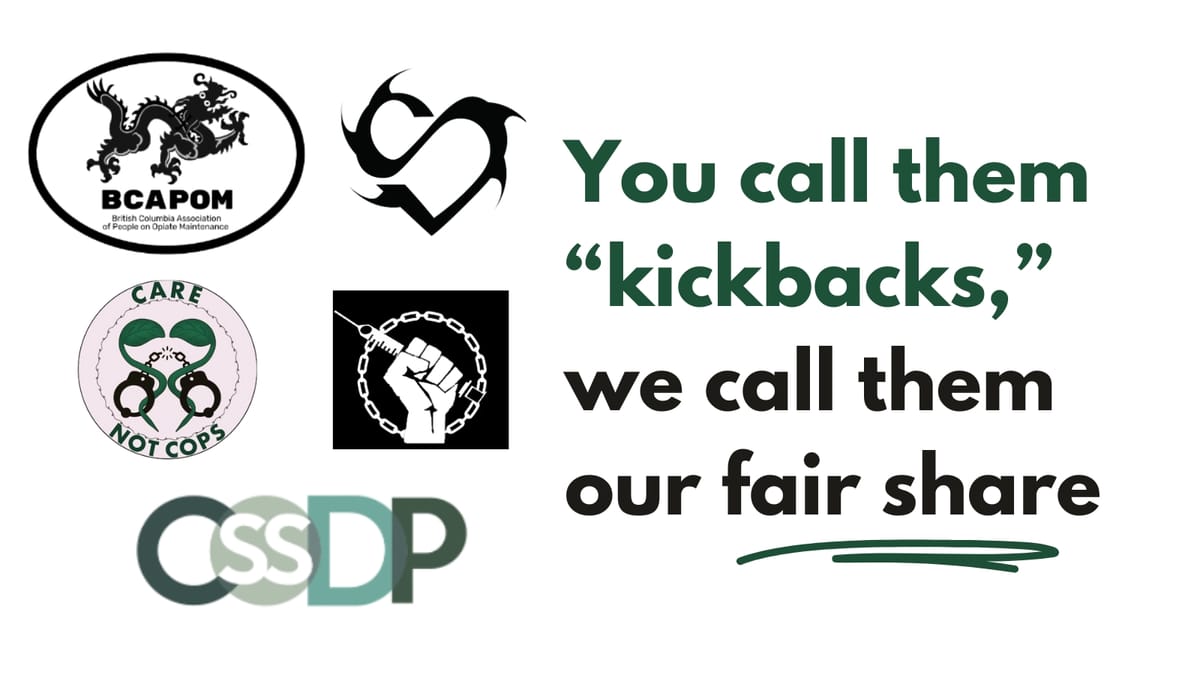
BCAPOM: You call them "kickbacks," we call them our fair share
The BC Association of People on Opiate Maintenance, Surrey Union of Drug Users, Care Not Cops, Canadian Students for Sensible Drug Policy Vancouver Chapter & Crackdown respond to recent coverage on pharmacy kickbacks, and the repercussions for them and the people they work with.
During the first overdose crisis in the 90s, cash incentives from pharmacies to people accessing methadone evolved alongside fee-for-service dispensing.
But with renewed media scrutiny, BC's Ministry of Health has cracked down on the practice – further marginalizing many kickback recipients who rely on them to make ends meet. People affected by the new rules are speaking out.
Two articles in March, one published by CBC and another by the Globe and Mail, brought renewed attention to pharmacy 'kickbacks' in BC’s lower mainland region. Kickbacks are a technically prohibited but longstanding, informal practice by which some pharmacies provide part of their profits from PharmaCare billing to low-income patients to incentivize filling prescriptions at their locations.
Following the media coverage, BC’s Ministry of Health issued a letter to pharmacies in Greater Vancouver that treat opioid use disorder in BC PharmaCare beneficiaries. The letter warns pharmacies of the harsh consequences of sharing cash incentives with their clients: an individual offering incentives could face fines up to $200,000 and/or six months imprisonment, while evidence that a pharmacy is sharing incentives could result in administrative penalties up to $50,000 and cancellation of the pharmacy’s enrolment in PharmaCare.
Since the warning was distributed, multiple pharmacies have abruptly stopped providing kickbacks to clients, many of whom rely on this income.
“Without my kickback, I can’t live.”
We were well aware that the media coverage in March would worsen conditions for us and the people we work with, while failing to meaningfully address the issues outlined in the articles. Among these are irresponsible pharmacy practices such as false dispensations. Meanwhile, at the root of the issue, as Dr. Lisa Howard stated to the Globe and Mail, “people living on the margins of society don’t actually have enough money to live.”
Now, people already struggling to make ends meet while surviving on paltry income assistance, disability and pension rates are faced with further financial hardship. At weekly meetings of the British Columbia Association of People on Opiate Maintenance (BCAPOM) in Vancouver’s Downtown Eastside (DTES), members report greater difficulty purchasing groceries and other essentials. Members have also expressed concern that the sudden reduction in income could force people to pursue criminalized income-generating activities, and that the increased financial pressure is resulting in increased tensions and lateral violence within our community. It is also more than likely that cutting off these payments will impact many patients' ability and desire to stay on their medications. Ultimately, this abrupt cutoff is a destabilizing force in people’s lives.
Kickbacks are a sliver of money given to people living in poverty – people navigating a time-consuming and stigmatizing medical system – a sliver of money out of a huge pie maintaining this unjust system.
"What’s the big deal if they want to give the customer a hundred dollars out of the thousands they are making off us? It’s the least they can do. I deserve that little bit of money. It wasn’t much but it made a big difference to me." -M, BCAPOM member who was recently cut off.
“Without my kickback, I can’t live.”
Kickbacks are not a new practice. They emerged during the first overdose crisis of the 1990s with the introduction of a fee-for-service system meant to encourage pharmacies to dispense methadone. As media coverage outlines, pharmacies dispensing medications to eligible low-income patients can bill PharmaCare daily fees of $10 for up to three medications. For witnessing patients taking their opioid agonist treatment (OAT) or methadone, pharmacies can bill an 'interaction fee' of $7.70. This means pharmacies can bill more than $1,000 per patient every month. Low-income people on daily witness OAT and other co-dispensed medications are a highly profitable patient population, leading pharmacies to compete for clients by offering a portion of these profits: a kickback.
J, another BCAPOM member adds, “We’re cash cows. They compete for us.”
A 2023 study found that daily witnessed OAT ingestion results in more than $30 million in excess expenditures every year in BC compared with weekly or biweekly dispensation. Little evidence supports this resource-intensive practice that has helped earned methadone the nickname 'liquid handcuffs.'
While daily witnessed ingestion is commonplace for methadone and some other medications prescribed for opioid use disorder, it has been shown to negatively impact people’s ability to meet day-to-day responsibilities and is cited as a reason for quitting or avoiding OAT. It means patients have to meet with their pharmacy every day to be supervised taking the medications needed to stave off withdrawal symptoms and reduce or eliminate their reliance on the increasingly toxic illicit drug supply. Patients must earn the right to take medications home, which can be difficult or impossible to achieve.
Trying to maintain employment or visit your friends or family outside of town? Prefer to take your medication at a different time than your pharmacy is open? Rely on deliveries and they’re not showing up? Pharmacy closed? Daily witness means entire lives revolve around maintaining prescriptions. This significantly impacts people’s time, relationships, income, autonomy, dignity and ability to survive.
"We deserve a piece of the profits made off of us."
Recent news coverage on kickbacks, the response from the Ministry of Health, and resulting cutting off of patients from these payments have only further punished those navigating this punitive and failing system. Ultimately, the excess expenditures of $30 million public dollars for daily witnessed ingestion will go straight to pharmacies, with none of these profits shared with clients barely scraping by. Cost of living continues to rise while income-assistance rates stay put.
"The pharmacies are milking us, getting paid for dispensing our scripts, watching us take our meds. We deserve a piece of the profits made off of us." -G, BCAPOM member.
Pharmacies who retain full funding from the PharmaCare agreement and offer none to service users have a vested fiscal interest in reducing competition – a conflict of interest unaddressed in news coverage. Many of these non-incentive pharmacies also have issues related to discrimination, exploitation and distrust. A number of us, as service users and as healthcare workers, have relied on incentive-based pharmacies as they’ve been willing to go into spaces (such as encampments) when others have not. Many of them have a higher threshold for behavioural bans when new clients are transitioning onto a medication, unlike some pharmacies owned by the wealthiest class, including Galen Weston.
In 2013, a methadone patient interviewed during the last crackdown stated the following, reflecting many of our experiences:
“They are trying to get it so that you will go to those drug stores [larger pharmacy chain stores] as opposed to the ones that are smaller, ‘cause they’re the ones that are giving incentives. Why shouldn’t drug stores be able to offer whatever to get more customers? I think that only benefits people such as ourselves…an extra 10 bucks here and there…when you’re living below the poverty [line], you’re absolutely going to take it.”
Previous media attention to the issue of kickbacks in 2008 led to harmful regulatory changes from the BC College of Pharmacists and the College of Physicians and Surgeons. Back then, Dr. David Tu, also involved in the most recent stories, contributed to a hidden camera investigation into the practice by CBC News, effectively recording people in a healthcare setting.
While Dr. Tu complained that kickbacks are "hundreds of thousands of dollars that could be so much better spent," the fee-for-service structure went unchanged. Instead, in 2013 the College of Pharmacists prohibited pharmacies from providing incentives, and with the College of Physicians and Surgeons, prohibited methadone delivery services, leaving only those with special authorization for "severe mobility restrictions."
“Solo actors demanding reform without solidarity from those most impacted have put people in danger.”
Research shows these regulatory changes had damaging consequences. Restricting deliveries had a major impact on access to methadone, especially for those living in extreme poverty. It also had a negative effect on people’s ability to manage competing scheduling demands, leading to missed doses and interruptions in co-dispensed medications. Kickbacks, while sometimes accompanied by problematic dispensing practices, provided people with much-needed additional income to meet their needs and reduce reliance on illegal income-generating activities. At times, kickbacks gave clients agency in negotiating dispensation arrangements – echoing discussions at recent BCAPOM member meetings.
The prohibition of pharmacy incentives exacerbated people’s structural vulnerability and lack of agency, while making it harder to comply with methadone program requirements.
The switch from generic methadone to Methadose also occurred around this time. This had deadly outcomes that were thoroughly documented by Crackdown Podcast.
These changes occurred with little to no involvement of those most impacted.
Tyson Singh Kelsall, a registered social worker and PhD candidate in SFU’s Faculty of Health Sciences, refers to the "long history of those with power in the medical system experimenting with opioid users’ lives: from the forced change to Methadose, to the abrupt rollbacks of safe supply, and now helping strike down kickbacks. Adequate safety measures were not put in place before cracking down and destabilizing people’s delivery and fraction of income sharing.”
“Solo actors demanding reform without solidarity from those most impacted have put people in danger.”
The College of Pharmacists has purportedly been reaching out to healthcare workers and clinicians in Vancouver's DTES to discuss kickbacks. The College has not yet reached out to groups representing those most impacted, in spite of their knowledge of BCAPOM – an organization by and for people on opiate maintenance that has operated in the DTES for almost 25 years. As such, BCAPOM and the Surrey Union of Drug Users (SUDU) have emailed BC’s College of Pharmacists, Ministry of Health, and Ministry of Social Development and Poverty Reduction to request they meet with these peer-led advocacy groups.
BCAPOM, SUDU, Care Not Cops, the Vancouver Chapter of the Canadian Students for Sensible Drug Policy, and Crackdown Podcast, as well as individual signatories, came together following the coverage in March 2024 out of concern for the recklessness with which these stories were told. We sent a letter to the journalists involved in the coverage and the clinicians who were interviewed, outlining many of the same concerns we have stated here. We received no response from the clinicians we wrote, including Dr. Burgess, Dr. Howard, and Dr. Tu.
We still welcome a response and opportunity for discussion between these clinicians and representatives from SUDU and BCAPOM. We urge the BC College of Pharmacists, Ministry of Health, and Ministry of Social Development and Poverty Reduction to answer these organizations request for meeting as soon as possible, in the hope that these discussions can generate solutions that do not replicate and continue destabilization, violence and other harm to us and our communities.
To protect their identities, names of British Columbia Association of People on Opiate Maintenance (BCAPOM) members are abbreviated in this article.
If you are a patient in BC who has been cut off from receiving kickbacks, and/or are having issues with your prescriber or pharmacy as a person on OAT or prescribed opioids, please contact BCAPOM at bcapom@vandu.org, or find us on Facebook or Twitter. If you are located in Surrey and have used or are currently using drugs, join the Surrey Union of Drug Users in the fight to end stigma and discrimination against drug users in Surrey. To learn more visit SUDU’s website or find them on Facebook.