BC NDP are weaponizing drug law to cover their healthcare and housing failures: Nurses & healthcare staff
Eleven staff in BC’s healthcare system outline the realities of frontline care work, the toxic drug crisis and their concerns.

By (in alphabetical order): Bilal Bagha MD CCFP, Blake Edwards BScN student, Fraser MacPherson RN, Heather Tunold BSW student, Jennifer Conway-Brown RSW MSW, Kara Jo Schultz RSW MSW, Lee Gangbar RN, Madelaine Beaumont RN(c) MN student, Nesa Hamidi Tousi NP, Serena Eagland RN & Tyson Singh Kelsall RSW MSW PhD(c)
Seven people in British Columbia will die of toxic drugs today. Seven died yesterday. And seven more will die tomorrow.
In 2023, the majority BC NDP government implemented a three-year “decriminalization” pilot. The province requested permission from the federal government for this as part of a purported response to stem the harms of the drug toxicity crisis.
In the 15 months since, despite it being one of the few substantial steps they had taken on the public health emergency, the BC NDP have backtracked on the pilot. They are instead re-criminalizing possession and use of substances in public, including the healthcare settings where we work. The BC NDP is reinvesting in a framework that continues to kill people in British Columbia at rates that have driven a prolonged, eight year public health emergency.
As nurses and healthcare workers, we view the BC NDP decision to recriminalize the public possession and use of unregulated substances as deadly and violent. We argue that the BC NDP and other actors have weaponized and obscured our colleagues' concerns to scapegoat people who use drugs and provide cover for their own failures of governing over the healthcare system, housing security and addressing poverty.
Some coverage of our workplaces in particular has been outright egregious and inaccurate.
We have been working on the frontlines of the toxic drug emergency in communities across the province. We witness firsthand the myriad ways that drug law has ravaged our communities. We witness the enormous loss of human life and other acute harms from the toxic drug emergency and drug war. We have lost clients, patients and loved ones to a preventable cause. Both our experiential knowledge and an established history of research has demonstrated that prohibitionist policies have devastating outcomes.
The crisis has been racist and settler colonial in its violence. For example, First Nations people in BC continue to die at extremely high rates from overdose, which contributed to a 7.1 year decrease in life expectancy across the First Nations population between 2015-2021. Desegregated, race-based data is not maintained by the province as part of the overdose response, but independent analysis shows that South Asian men also disproportionately die from the crisis in the Fraser Health region, which includes Surrey.
Institutional abandonment
We condemn the silence of our health and social institutions as the BC NDP toys with the lives and rights of people, including people we care for, and produces policy that will negatively impact public health outcomes in general.
Health authorities and the British Columbia Nurses Union have either stood by in silence, or worse, engaged in this active campaign against the public they should be providing care for, part of the organized abandonment and dehumanization of people most impacted by the poisoned supply.
Let us be clear: the use of substances is not a safety concern in our workplaces. But the denial by all levels of government to undercut the contaminated drug supply is.
Realities of drug use
In many cases, witnessing someone consume a substance is a relief, knowing they are doing so in a setting where an overdose response is at the ready, and that their pain/withdrawal symptoms are being met in ways that the medical model remains unable and unwilling to.
As clinicians who rely on scientific knowledge, we recognize there is no real risk to witnessing use or touching fentanyl. With the absence of safe inhalation sites, we also understand why our clients may use substances indoors at times, particularly when pain and withdrawal is inadequately or poorly managed. As clinicians, researchers and educators, we recognize that vapours produced during fentanyl inhalation do not pose a health risk to those within the vicinity of the user.
Workplace and residential research from New Zealand and the US also shows no long-term health impacts from brief airborne or surface exposure to crystal methamphetamine. There are mild short term effects such as throat irritation and watery eyes, but crystal methamphetamine does not accumulate in the body, so long-term implications are highly unlikely.
Witnessing someone consume substances is not a threat to the safety of workers or to the public. But when drug users are coerced into using in secret or alone, the rate of fatal toxic drug poisoning increases dramatically. And 70-85 percent of overdose deaths continue to occur in private residences each month.
In this crisis context, people contend with extreme withdrawal symptoms caused by complex mixes of opioids, benzodiazepines, tranquilizers, and other unknown cutting agents more extreme than previous eras of drug use.
Our medical system does not keep up with this shifting drug supply, which will continue to change under our prohibitionist policies to evade law enforcement crackdowns. And while Suboxone prescriptions and Sublocade injections can have benefits for some, they are not appropriate or therapeutic replacements for the majority of people who rely on the current unregulated opioid supply after hospital admission.
A public health approach to poisoned supplies of any other kinds – food, alcohol, water, etc. – would come with new regulations and processes to stop the poisoning. We would not just send people to the emergency room indefinitely. Ultimately, this shows that the current direction is not about reducing harm, but rather to disappear drug use(rs) from public life to isolated areas.
As healthcare workers, we stand behind our rights to workplace safety – and drug use is not a threat to this. There are solutions to the harms that are being caused.
Earlier this month, Saint Paul’s Hospital in Vancouver opened a safe inhalation site for patients, which saw over 200 visits in its first week.
If the drug supply was predictable and regulated, people would have more autonomy over dose, location and timing of their drug consumption, or whether to use at all. But the current toxic supply makes managing withdrawal symptoms incredibly difficult for those reliant on it. An accessible, non-prescriber drug distribution model, as recommended by BC’s own expert Death Review Panel, is in all of society’s interest.
David Eby's NDP are obscuring the crisis
The BC NDP’s constant amending and abrupt dismantling of decriminalization has come without consultation with people impacted or education to the public. The result is a collection of policies that cause confusion and create conflict in the field.
Decriminalization is not the only way the BC NDP have turned the drug toxicity crisis into a public relations tool they seem intent on gambling with for electoral gain. A political gamble, even though Health Canada’s 2022 poll showed only four per cent of people in BC believe a primary focus on police enforcement is the right approach to the crisis.
Rather than addressing the drug supply directly, the Eby-led NDP have conflated the public health emergency of a poisoned supply with loosely related funding decisions, including to float involuntary treatment, fund private recovery programs without measured outcomes or fatalities, and blame drug users for all forms of public disorder.
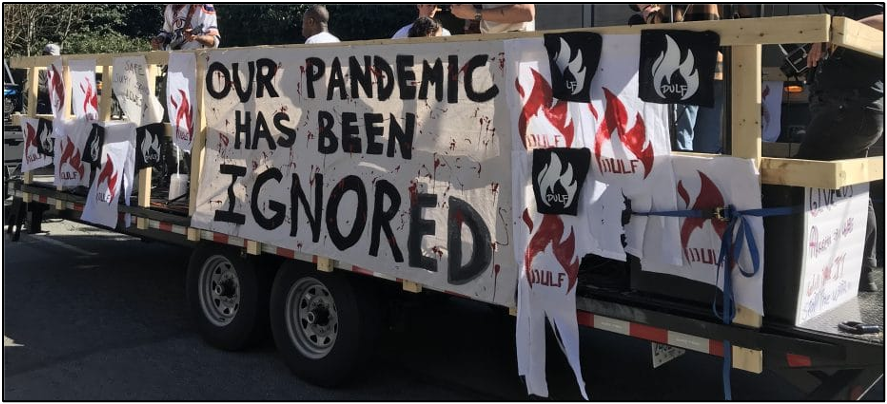
Relative to the COVID-19 pandemic response, the drug toxicity crisis has not received dedicated attention from the BC government. There has been a notable absence of provincial health officer intervention, while the emergency orders that do exist have not been followed. We know a different form of resource mobilization is already possible.
The Death Review Panel conservatively estimates that 225,000 people in British Columbia use unregulated drugs, and less than half of that number would meet criteria for a disorder. As such, the majority of people who use unregulated substances are not eligible to receive a prescription for regulated stimulants or opioids. Framing this emergency as solely a healthcare system or criminal justice issue fails to acknowledge that drug use is, at its root, one of many human behaviours whereby risk of death should not be a normalized consequence.
Panic pre-dated decriminalization
The public panic over use in hospitals and healthcare sites is not only overblown, it is dangerous. People who use drugs already struggle to stay in hospitals for many reasons, from the lack of an adequate replacement supply to intersecting forms of discrimination. Creating more reasons for premature discharge will result in more premature death.
From the very start, the model for BC’s decriminalization pilot was criticized for not clearly reducing the criminalization of drug possession and use(rs). The model is littered with exceptions, and it provides new discretion, tools, and resources to police. This has made the policy difficult to understand and implement. In at least one jurisdiction, raw counts of drug seizures seemed to have only increased, reflecting the significant growth in police budgets across the province.
Rather than scaling up to adequately decriminalize drug use and render the model useful, the BC NDP continue to use drug law as political theatre to cover for their failures after seven years in power: from Surrey’s primary hospital being at constant risk of closure to driving up housing insecurity for those precariously housed.
All of these realities impact the health of our patients, as well as our own practice.
And all this panic was manufactured prior to decrim even starting. The BC Association of Police Chiefs highlighted as much in their letter to government during their successful resistance to the plan of 4.5-grams of drug possession being decriminalized (countering consultation from communities who are impacted by these ever-changing policies). The municipality of Campbell River attempted to pass a consumption ban the day decrim was set to start, although they struck it down after Pivot Legal Society announced a legal challenge.
Decrim has been extremely limited in scope, and the surrounding harmful panic was embedded in its public relations, which follows a long history of unreasonable mainstream discourse surrounding drugs.
HRNA Charter Challenge
The BC NDP’s latest move to re-criminalize drug possession side-steps a pending Charter challenge from the Harm Reduction Nurses Association on a public consumption ban they previously tried to pass via Bill 34.
We all strongly support HRNA’s legal challenge.
Bill 34 was a legislative process that was halted by a temporary injunction based on its potential to cause irreparable harm. Bill 34 has been criticized or opposed by wide-ranging groups, from the Union of BC Indian Chiefs, the BC Civil Liberties Association and the BC Association of Social Workers to drug user groups, including the Surrey Union of Drug Users and Eastside Illicit Drinkers Group for Education.
In a statement to Drug Data Decoded, HRNA president Corey Ranger writes, “Bill 34 will drive isolated drug use and death. It will keep none of us safe. Our lawsuit is a plea to the government to use the tools we know it has…Let’s channel our anger toward those who have the power to make a difference.”
Bill 34 targets people who use drugs on its face, but is embedded with a reckless increase in police discretion against people that officers believe recently consumed a substance – a tool history tells us will be weaponized against those living outdoors, Indigenous Peoples, sex workers, and/or racialized and otherwise marginalized individuals and communities. But the temporary injunction won by HRNA in December 2023 forced important context about the drug toxicity crisis into the legal system – including the myriad of harms caused by forced displacement and police interactions.
“As our clients and loved ones continue to die in record numbers, BC has refused all reasonable approaches and opted for a punitive law that, quite simply, will not be effective,” added Ranger.
Seven people will die today of toxic drug poisonings, and more people will die tomorrow, due to the impacts of prohibition and criminalization. Every premature and preventable death is the result of policy choices. The drug toxicity emergency deserves an urgent and adequate response.
You can read a follow-up solidarity statement & and you can sign on here.