Did drug poisonings drive the ambulance crisis?

Massive ambulance shortages in 2020 and 2021 threatened the collapse of emergency health services and dominated the news.
The story that was never told: how the ambulance crisis was likely both a cause and effect of unmitigated drug poisoning.
Remember Betty Ann Williams, the Calgary woman who perished in June 2022 after being mauled by dogs and waiting half an hour for an ambulance to arrive.
The noise made by Alberta's paramedics union about "running out of people to do the work."
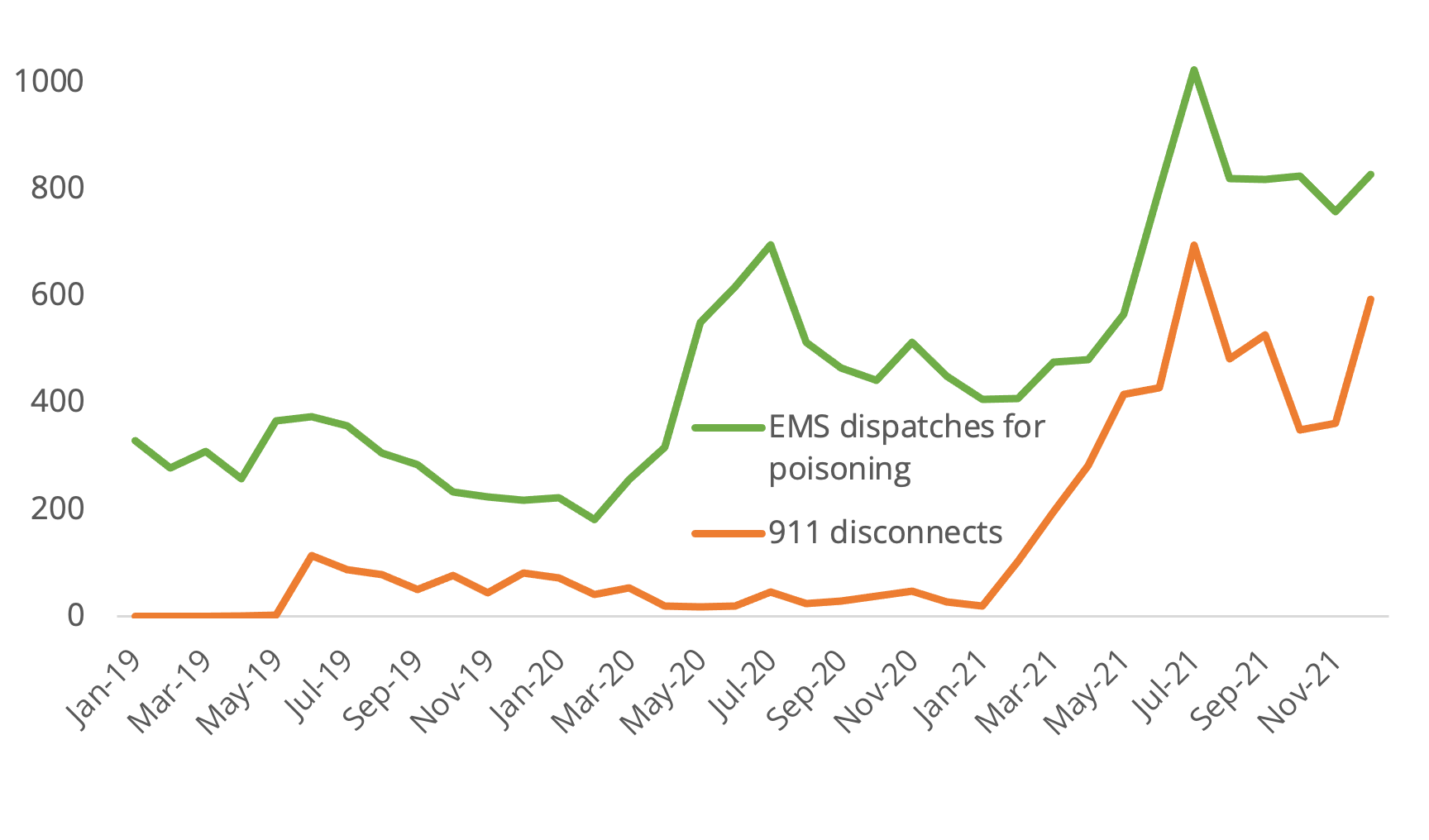
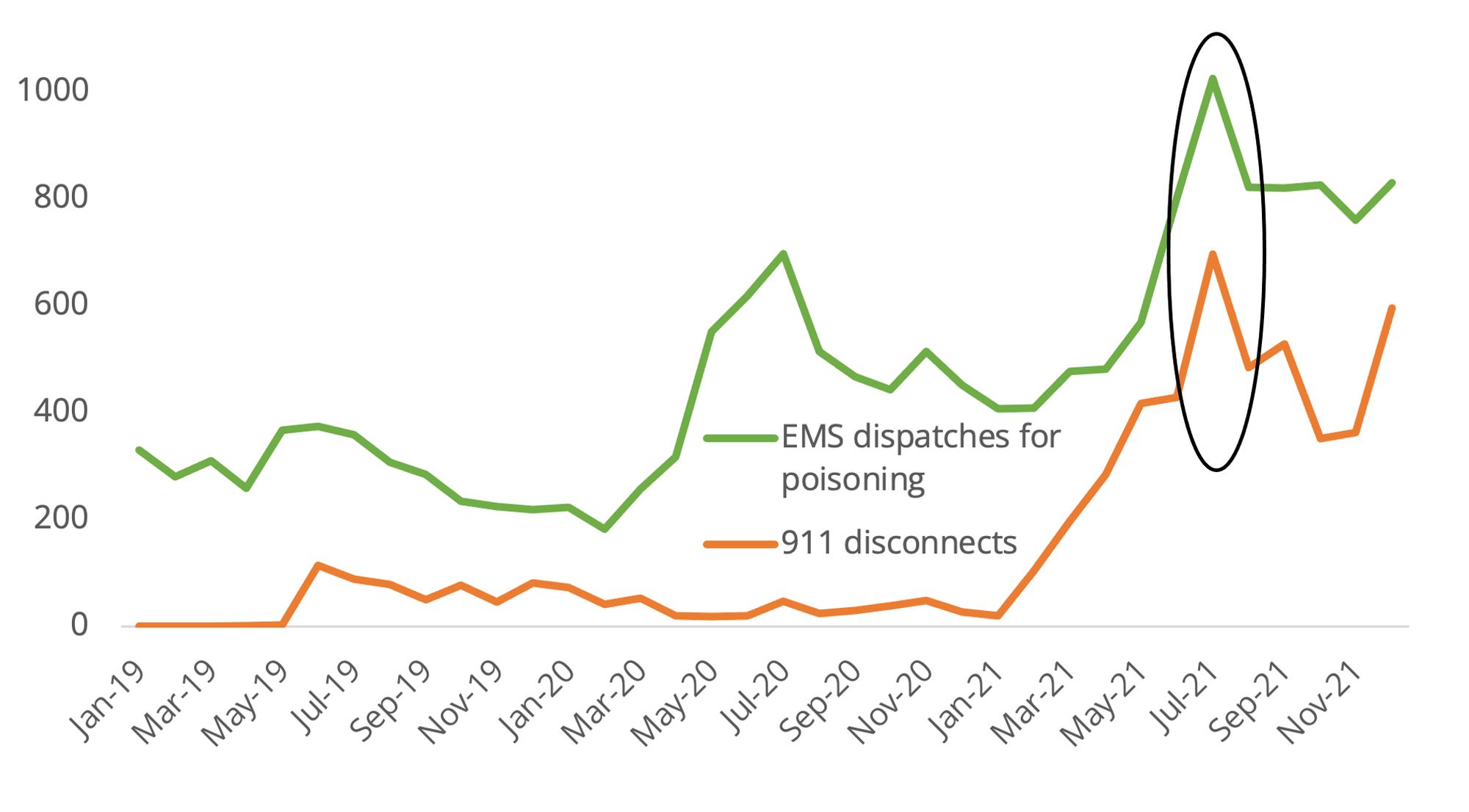
Through 2021, ambulance red alerts (when capacity is maxed out) broke records while 911 dispatchers began hanging up on people with less urgent emergency calls to direct resources to the most serious calls. It turns out, unregulated drug poisoning may have driven this crisis to a degree not previously discussed in media.
Data obtained through a Freedom of Information request and reported in February 2022 by CBC's Rob Easton revealed the extent of the ambulance crisis experienced in Calgary and Edmonton through 2020 and 2021. July 2021, the first month of the Alberta government's ill-fated "Best Summer Ever," coincided with record-setting EMS dispatches for drug poisoning.
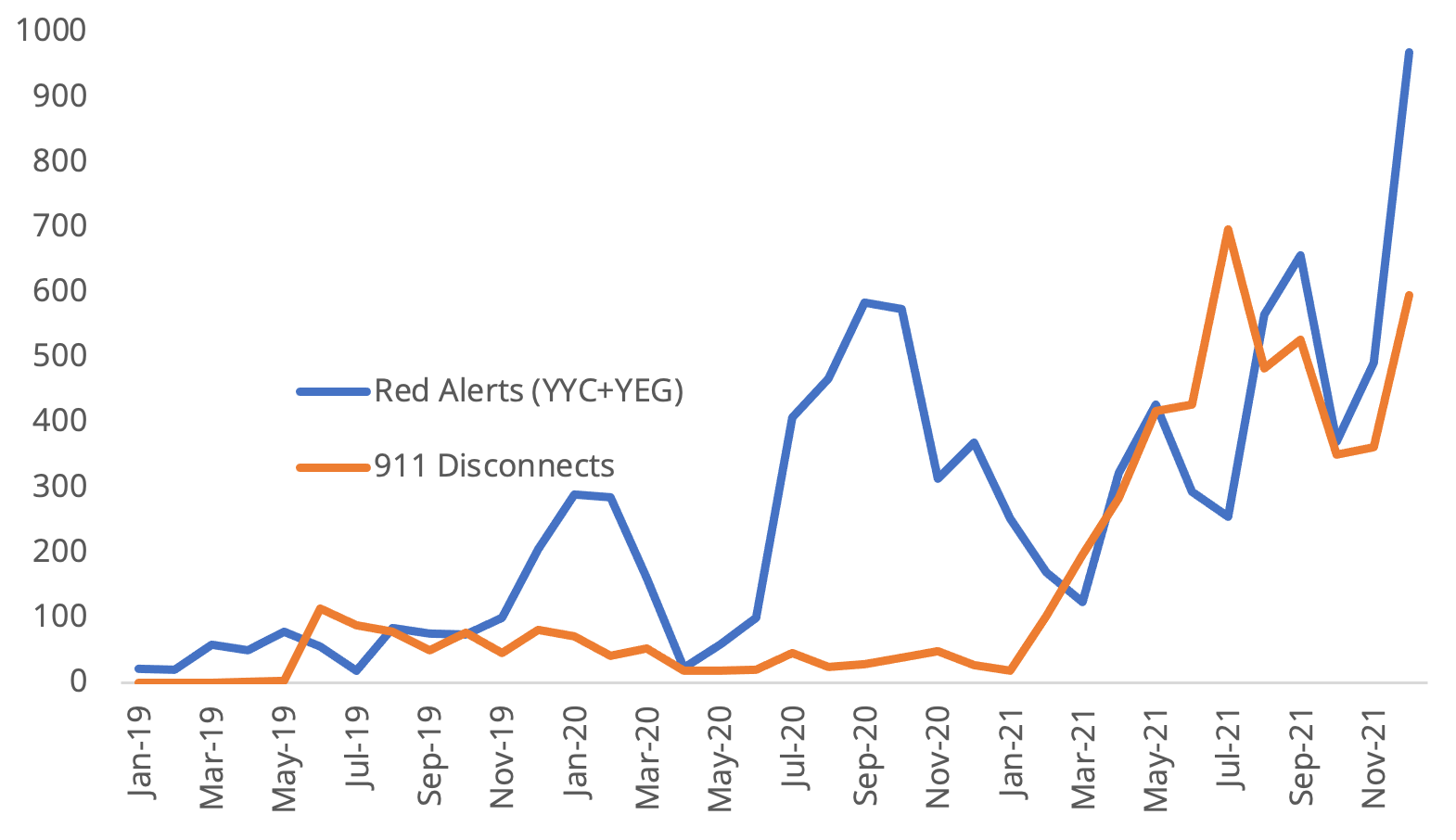
911 disconnects correlated very tightly with spikes in drug poisoning EMS dispatches, which suggests that drug poisonings were triaged as high-priority calls. This also means people were likely disconnected from other 911 calls as a result of high drug poisoning rates.
This could situate unregulated drug toxicity near the centre of emergency health care collapse in Alberta. Consider Edmonton ICU physician Darren Markland's perspective from a CBC story published in July 2023:
"I have never seen so many opiate overdoses and out-of-hospital cardiac arrests as a result of drug poisoning in my entire life, and that's saying something for a doctor who has worked 20 years in an inner city hospital...People are dropping dead on the streets."
In the same story, an [at the time] unhoused community member named Marshall Dines told CBC: "I've Narcanned four people this week and I've watched a couple pass away." (Narcan is a brand name for naloxone, an antidote that reverses opioid poisoning.)

It's not only that increases in EMS dispatches for drug poisoning are proportional to increases in 911 disconnects. The magnitudes are sometimes very close. For example, while EMS dispatches for poisoning increased by 224 between June and July 2021, 911 disconnects increased by 268. This could mean that 224 of the 268 911 disconnects that month were a consequence of unregulated drug toxicity stretching the system past its capacity.
This heavy impact of unregulated drug poisoning could in part reflect what transpires when EMS is dispatched to these situations: depending how frequently they are fatal, dispatches can turn into transport of the person to the morgue for medical examination.
But not all are fatal, and even non-fatal EMS dispatches can take considerable time when the patient is disoriented or unsure about whether to accept transport to the hospital.
What explains these jumps in EMS dispatches for drug poisoning–and the extreme pressure it appears to place on emergency health care?
It turns out, EMS dispatches for drug poisoning also correlate tightly with the frequency that people experience drug poisonings under supervised consumption at Calgary Safeworks.
This makes sense: when people bring drugs into the site to consume, staff are there to respond when a poisoning happens–as often as 8 of every 100 uses of the site. When the toxicity is higher in drug supplies across the province, more poisonings are recorded under supervised consumption–and more poisonings are attended to by paramedics.
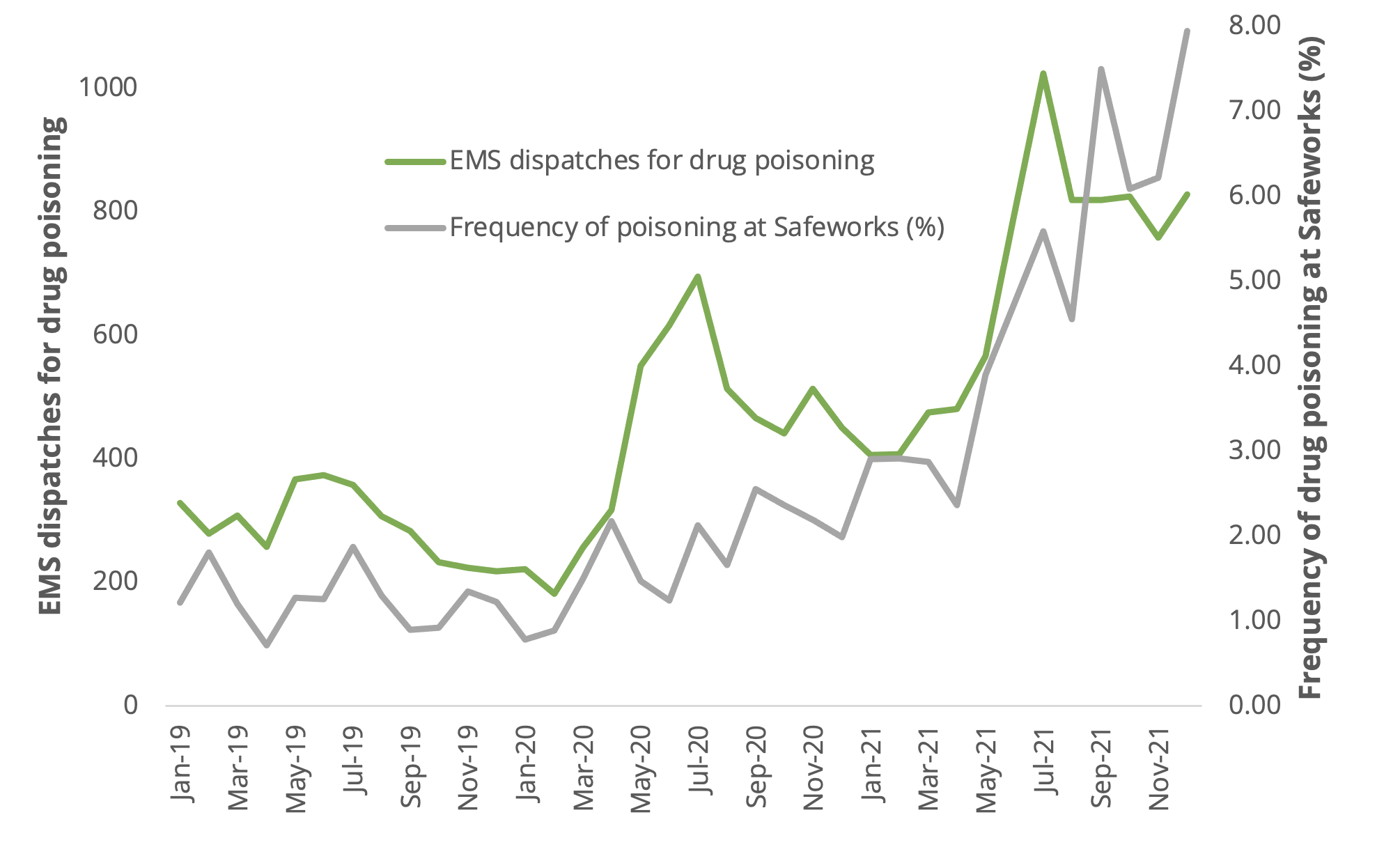
The frequency of poisonings during supervised consumption site visits ebbs and flows, sometimes rising to 8%, and provides a rough estimate of how frequently people outside of these sites are experiencing poisonings. As people get used to supply changes or as the supply reverts to lower toxicity (lower fentanyl concentration or lower presence of adulterants like benzodiazepines), the poisoning frequency returns to a lower level. Pre-pandemic, it was normal to see around 1-2% of site visits result in a poisoning.
The staggering increase in drug supply toxicity indicated by the frequency of drug poisonings at Safeworks through 2021 matched a dramatic rise in both red alerts and 911 disconnects.
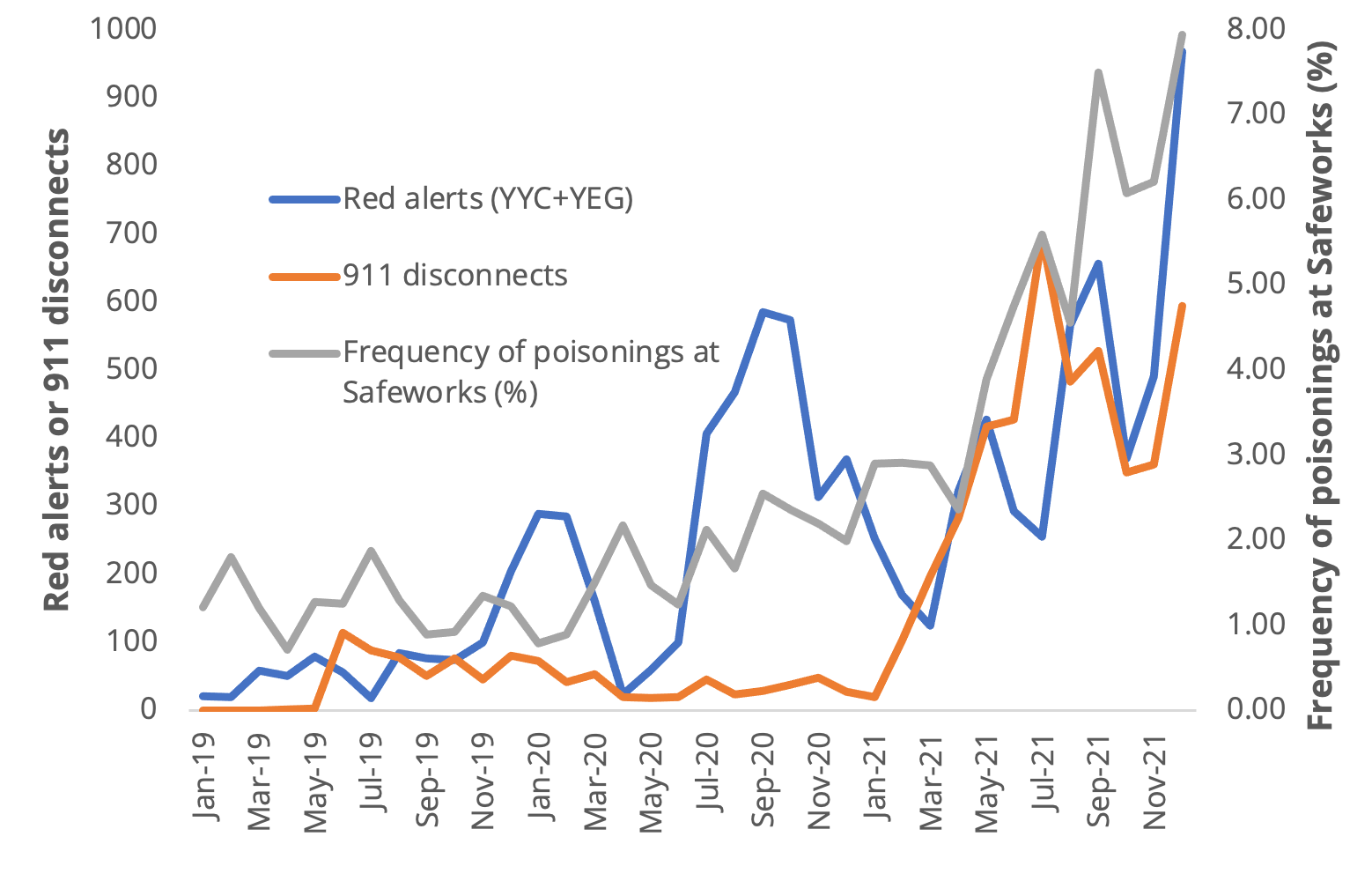
If increases in drug supply toxicity trigger more EMS dispatches, and these in turn result in more red alerts and more 911 disconnects, we can link unregulated drug supply toxicity directly to the crisis in emergency health care. People in all kinds of medical emergencies are left waiting for ambulances–or left hanging on a dead phone line–as a result of unregulated drug supply volatility.
How many people died of unregulated drug toxicity–the leading driver of reduced life expectancy in Alberta–while waiting on a delayed ambulance?
Ironically, while these convergent ambulance and drug poisoning crises were reaching a crest in December 2021, the UCP government was busy passing a motion to establish a Select Special Committee to Examine Safe Supply. This delivered its final report in April with a predictable verdict: Alberta must double down on abstinence-based treatment and avoid safe supply.
Meanwhile, BC's safe supply programs were just beginning to release data. The latest study shows up to 91% reduction in week-to-week mortality among people accessing regulated hydromorphone.
And it would not be a stretch to suggest that unregulated drug poisoning has been harnessed by the UCP government to collapse public health care and clear the way for increased privatization.
Subscribe to Drug Data Decoded
If you find this work useful, please consider subscribing or sharing with a friend.