Up to 89 percent of ambulances for overdoses concealed in record year, as Alberta health care careens into crisis
The Alberta government says it has “the most transparent data reporting system in North America" for drug toxicity. In reality, internal data manipulation causes most emergency calls to go unreported.
UPDATE, February 26, 2026 – the Alberta government has reacted to this story with a notice on its public dashboard. See bottom of story for details.
For years, the Alberta government has claimed its Substance Use Surveillance System is “the most transparent data reporting system in North America.”
But Alberta Health Services (AHS) documents obtained by Drug Data Decoded reveal that this 'transparency' had a caveat: most ambulance dispatches for drug toxicity are concealed in the government's public-facing reports.
The documents, detailing EMS dispatches for all emergency types in the month of February for 2024 and 2025, show that in February 2025, 89 percent of EMS dispatches for drug toxicity in Calgary were not reported by the government.
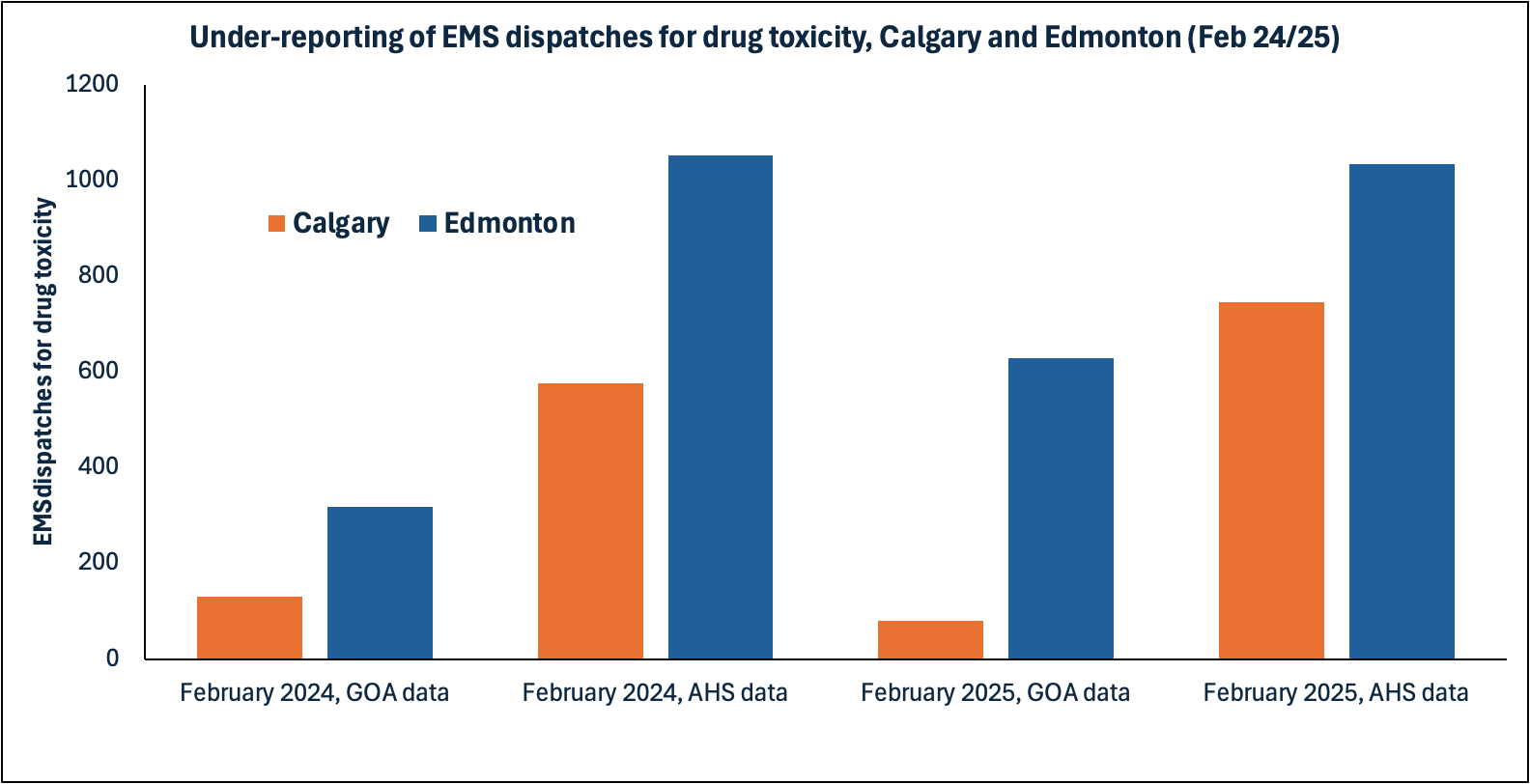
This pattern also played out with provincial data, obtained in a separate freedom of information request from AHS for 2020 to 2023. In each year, between 70 and 85 percent of provincial EMS dispatches for drug toxicity ("Card 23" events) were not reported by the Alberta government.
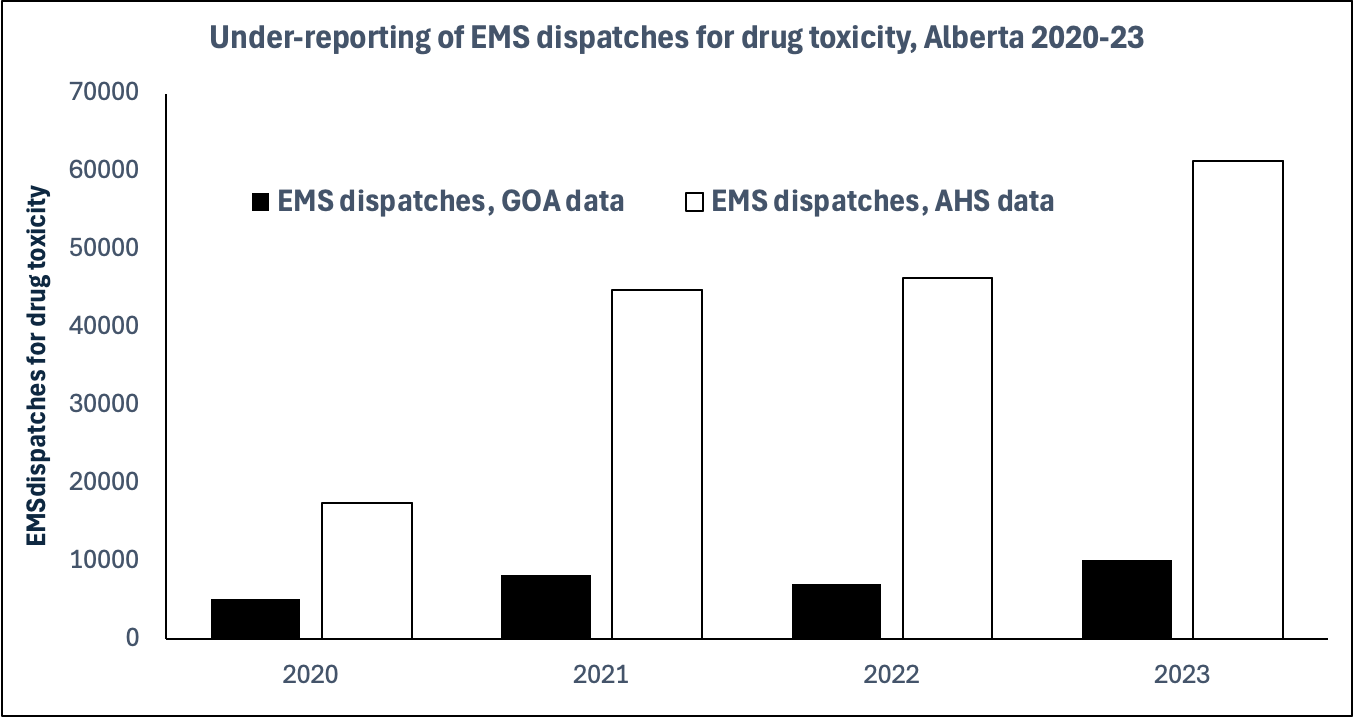
In its reporting, the Alberta government shows "EMS responses to opioid related events," without revealing EMS responses for any other type of drug poisoning event. These data contain two obvious discrepancies that drive under-reporting of the total EMS dispatches for drug toxicity: the first, that non-opioid drug toxicity events contribute significantly, but are not included in the public reporting; the second, that no combination of opioid-related dispatch codes from the AHS data appear to add up to what is reported by the government.
A further factor that likely deflates even internally reported dispatch figures is the information provided to dispatchers by first responders. Angie Staines, a nurse who runs 4B Harm Reduction in Edmonton, says that many overdose response trainings emphasize not reporting the presence of drugs, instead focusing on "respiratory distress" while informing the dispatcher that the responder is carrying and administering naloxone.
Staines also emphasizes that responder safety needs to carefully assessed while calling for help: "If there's no violence, do not give dispatchers a reason to think there is."
A Calgary nurse who also trains people on drug poisoning response said, under condition of anonymity for fear of reprisal, that "because there is a high chance that cops will show up if you say it's an overdose and not just an unconscious person," responders often avoid mentioning drugs to dispatchers. This is important because of the abuse of the Good Samaritan Act by authorities, including the wrongful arrest and conviction (overturned) of Saskatchewan resident Paul Eric Wilson during a drug poisoning he attended to in 2020.
Indeed, calls for "Unconscious Fainting − Not Alert" and "Unknown Problem (Man Down) − Life Status Questionable" increased nearly 100-fold and 12-fold between 2017 and 2023, with peaks and valleys correlating closely with those of EMS dispatches recorded for drug toxicity, but not with dispatches for difficulty breathing (as might be expected if they were driven by COVID or flu responses). This could represent tens of thousands more drug toxicity dispatches going unreported.
On January 14, Drug Data Decoded asked Alberta's Ministry of Mental Health and Addiction how it arrives at its reported numbers, and whether it believes that the increase in dispatches for 'unconscious fainting' and 'unknown problem' are a result of criminalization of first responders to drug poisonings. The ministry did not respond.
The British Columbia Emergency Health Services publicly reports all "Card 23" events, meaning all drug toxicity events, and these match those in the obtained AHS datasets. The data reveal that Alberta had a lower number of EMS dispatches for drug toxicity than BC in 2020, but a higher number of dispatches than BC for 2021, 2022, and 2023 – by margins of 26, 35 and 46 percent.
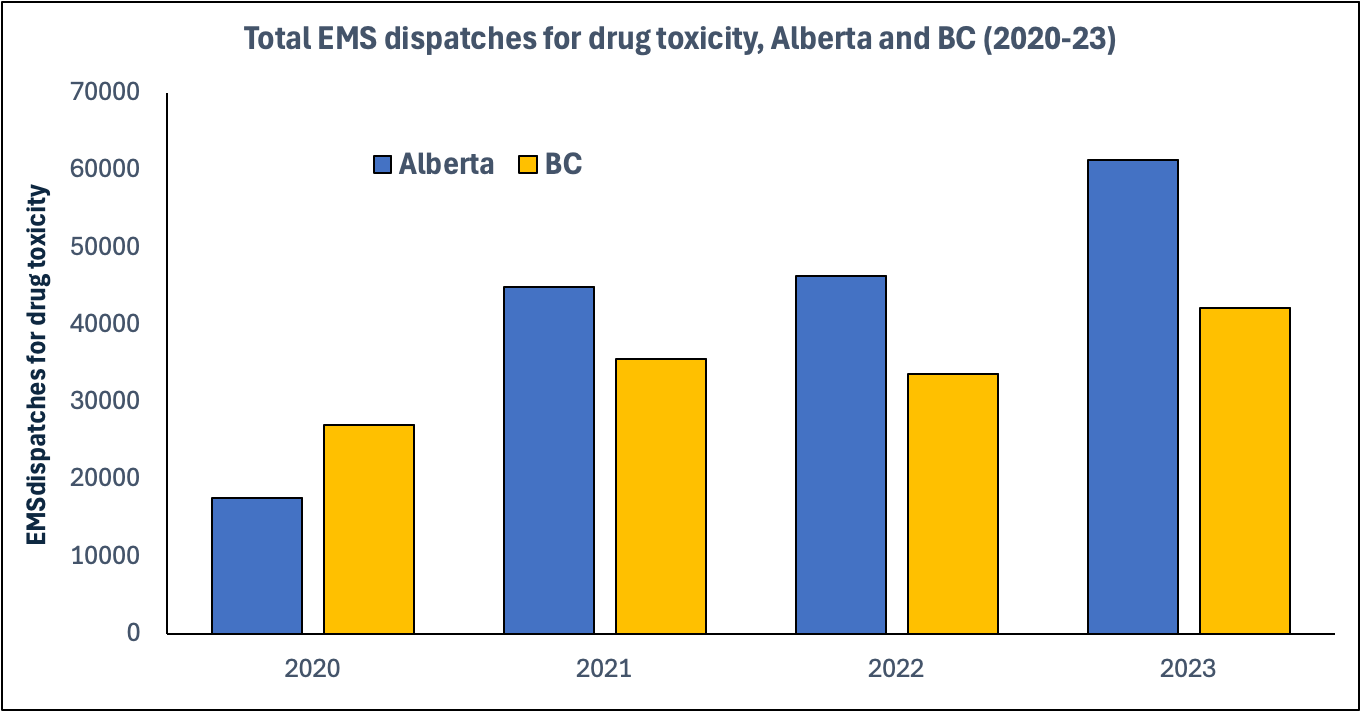
The Alberta government frequently compares its incomplete fatality data to the more complete data reported by the BC government, and has leveraged those unsupported fatality differences to advance its abstinence-focused policy agenda. In Alberta, official fatalities tend to creep upward by 20 to 30 percent after their initial announcement, while in BC, fatalities only increase by around 10 percent.
EMS dispatches and fatalities for drug toxicity are tightly correlated, as revealed by Drug Data Decoded in 2023. BC continues to show higher fatality counts than Alberta in each of these years, but reports data more quickly through its provincial coroner service. Analysis of the Cause of Death dashboard reveals that Alberta still has 3,244 fatalities pending investigation by the medical examiner from 2020 to 2024. Most of these are from 2022 (518), 2023 (1,244), and 2024 (1,218).
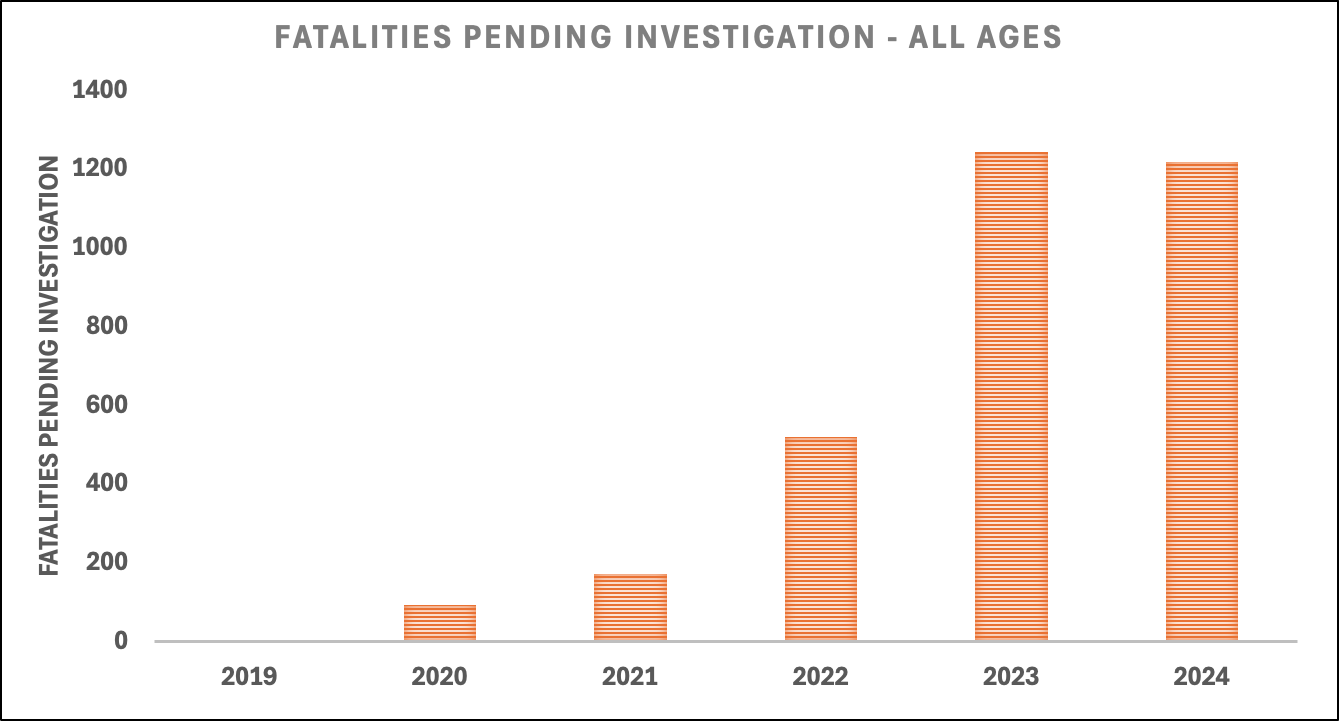
Roughly 40 percent of the fatalities pending investigation are for ages 18 to 44, the age group most heavily affected by drug toxicity. Alberta's Chief Medical Examiner insisted in 2025 that the fatalities pending investigation will not affect drug toxicity statistics, but updates are continually made to drug toxicity deaths from previous years. In recent months, updates have been made to fatality statistics in 2022 and 2023.
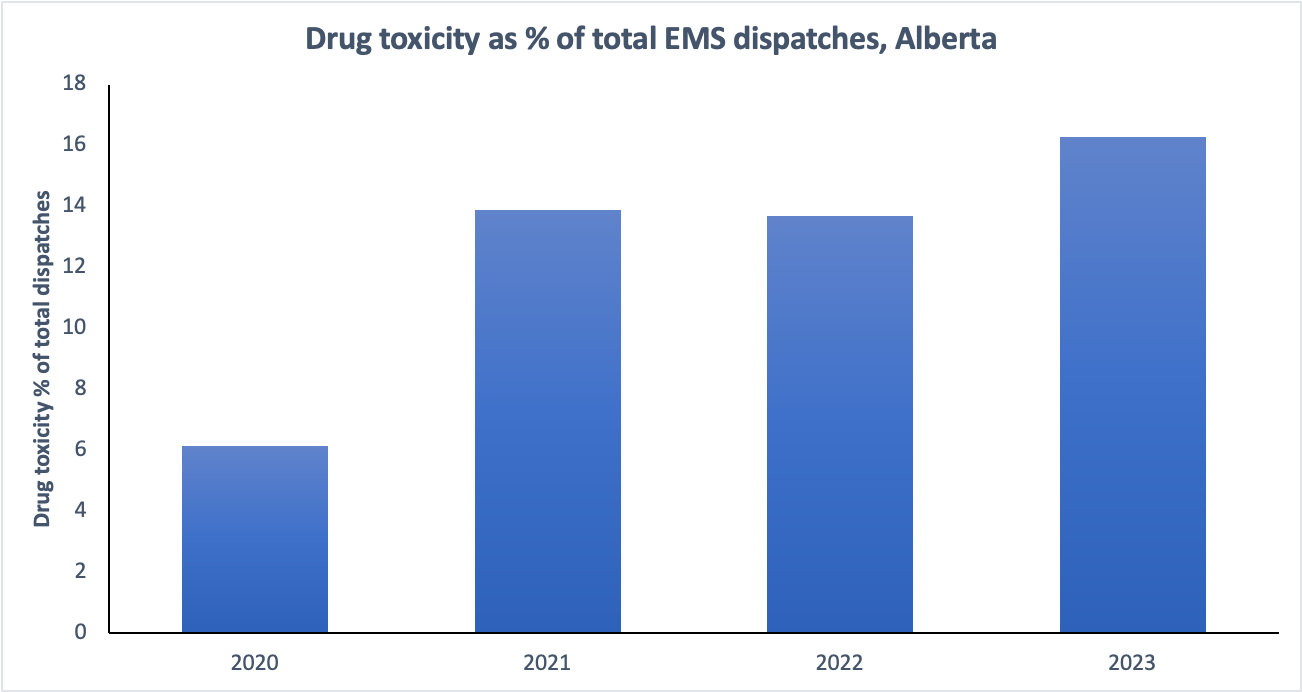
These data reveal that the crisis of emergency rooms running over capacity is likely being aggravated by inaccurate data being presented to the public and to health care decision-makers. Recent media reports indicate that deaths are occurring in emergency rooms while patients wait for care, and emergency room physicians are sounding the alarm.
Between 2020 and 2023, the AHS data show that drug toxicity made up an increasing fraction of the total EMS dispatches, rising from six percent to over sixteen percent. This means that the collapse of health care services in Alberta is due in no small part to the province's unwillingness to address the toxic drug supply while it continues pouring billions of dollars into its abstinence-focused 'recovery-oriented system of care.'
Emergency rooms and paramedics aren't alone in this. Firefighters in Red Deer recently warned that their emergency responses for drug toxicity, which are not counted among the EMS dispatch data, have skyrocketed since the government closed the supervised consumption site in the city. The government denied a link between the site's closure and the 51-percent year-over-year rise in fire crew responses to drug toxicity.
For years, the crisis plaguing Alberta's streets and emergency rooms was tempered by the 40,000 drug poisonings managed by supervised consumption sites. While the Alberta government continues closing these services, EMS data reported for 'opioid related events' in Alberta for 2025 already shows it to be the worst year on record, with 10,648 dispatches translating to approximately 65,000 Card 23 events (total dispatches for drug toxicity).
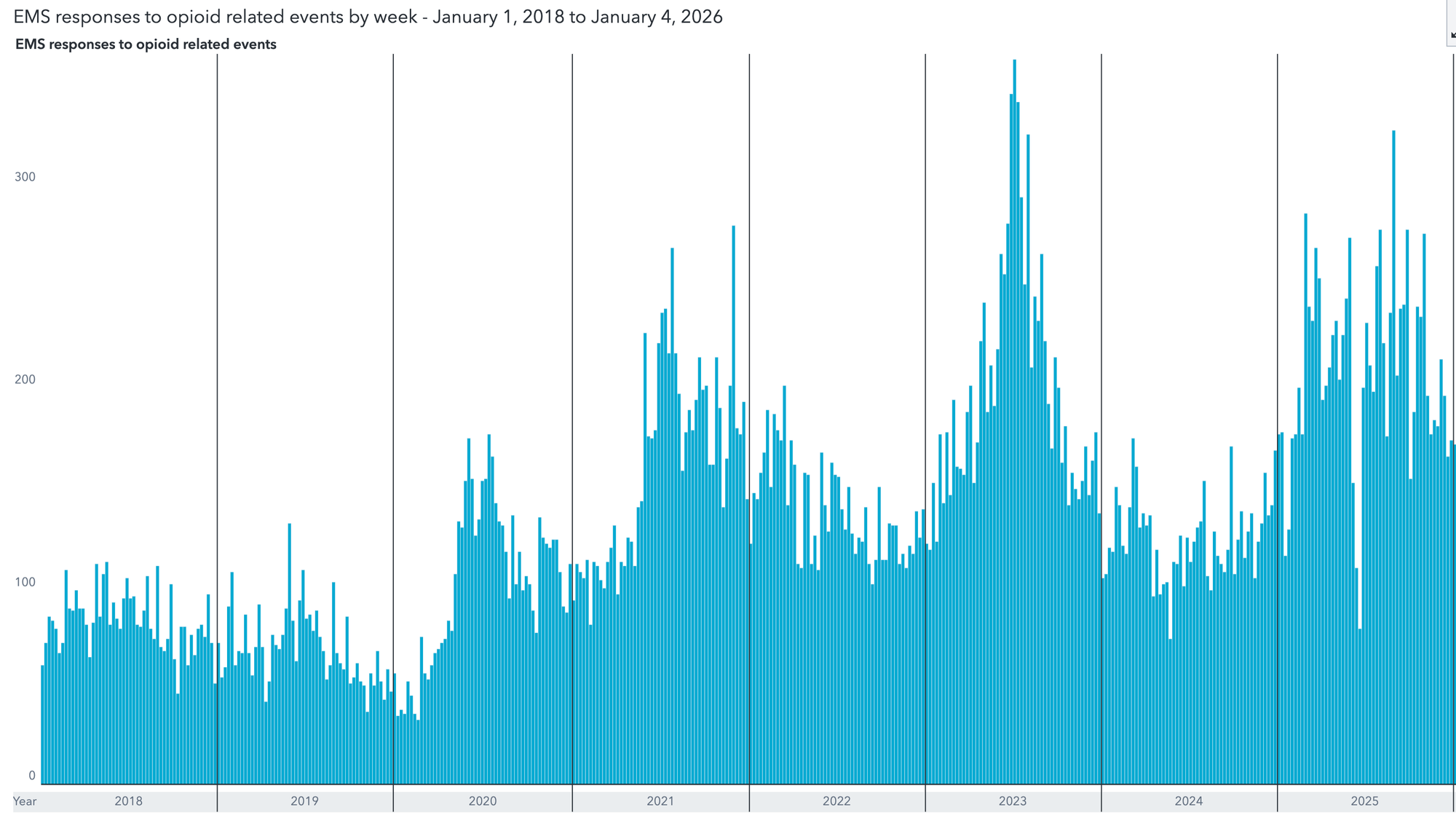
It will be years before mortality data are finalized, but the strong relationship between EMS dispatches and fatalities suggests that fatalities also broke the 2023 record in 2025.
As the province continues its assault on supervised consumption services, while defunding harm-reduction organizations like SafeLink in Medicine Hat and Turning Point in Red Deer, people in Alberta can expect a greater portion of EMS and hospital capacity to be consumed by the preventable fallout of the war on people who use drugs.
UPDATE, February 26, 2026: The Alberta government has adjusted its dashboard reports for "EMS responses to opioid-related events" to read the following:
Drug Data Decoded rejects the government's claim that its suppression of dispatch data creates greater accuracy in reporting. By only capturing the transfers of at hospitals, the Alberta government continues to obscure the following events from public reporting:
- EMS dispatches for drug poisonings not involving opioids
- EMS dispatches for opioid poisonings where Medical Control Protocol was not documented
- EMS dispatches where no naloxone was administered
- Calls for dispatch that are responded to by fire departments
- Calls for dispatch that are managed by outreach workers
- Calls for dispatch that are managed by community members
Drug Data Decoded further holds that the data strongly suggest many opioid-related dispatch events are not captured when the dispatcher records "Unconscious Fainting − Not Alert" and "Unknown Problem (Man Down) − Life Status Questionable," many instances of which are responded to by non-EMS citizens listed above.
Documents used in this reporting:
An early version of this story was shared with Paid subscribers on January 22, 2025.
Drug Data Decoded provides analysis using news sources, publicly available data sets and freedom of information submissions, from which the author draws reasonable opinions. The author is not a journalist.
This content is not available for AI training. All rights reserved.